Management of Neonatal Respiratory Distress Syndrome by Indigenous CPAP in a Resource Poor Setting
Vishal Pooniya* and NishaPandey
DOI10.21767/2471-805X.100001
Vishal Pooniya1* and NishaPandey2
Department of Pediatrics, King Georges Medical University, Lucknow, India
Assistant Professor, Department of Pediatrics, Rohilkhand Medical College, Bareilly, Uttar Pradesh, India
- *Corresponding Author:
- Vishal Pooniya
Lecturer, Department of Pediatrics, King Georges’ Medical University, Lucknow
Tel: +966 566 625 736
E-mail: vishalpooniya@gmail.com
Received date: September 11, 2015 Accepted date: October 06, 2015 Published date: October 25, 2015
Citation: Pooniya V. Management of Neonatal Respiratory Distress Syndrome by Indigenous CPAP in a Resource Poor Setting. J Pediatr Care. 2015, 1:1. doi:10.21767/2471-805X.100001
Abstract
Approximately 25% of the global neonatal mortality is contributed by India. Many high risk deliveries take place in resource poor settings. A preterm (35 weeks) male newborn delivered in a peripheral private hospital, with respiratory distress syndrome was managed by us using an indigenously developed continuous positive airway pressure (CPAP) circuit. This type of low cost CPAP device may be quite helpful in managing neonatal respiratory ailments in developing nations.
Keywords
Continuous positive airway pressure; Respiratory distress syndrome; Indigenous
Abbreviations
ABG- Arterial blood gas CPAP- Continuous positive airway pressure CRP- C reactive protein FiO2 – Fraction of inspired oxygen IV- Intravenous RDSRespiratory distress syndrome SpO2- Oxygen saturation of Hemoglobin
Introduction
Continuous positive airway pressure (CPAP) has been shown to reduce the need for mechanical ventilation. In resource poor settings that are quite prevalent in our country, indigenously developed low cost CPAP devices can be very helpful in lowering the neonatal mortality. We herein describe a preterm newborn with respiratory distress syndrome (RDS) managed with the help of an indigenous nasal CPAP circuit.
Case Report
A preterm (35 weeks) male newborn was born out of a nonconsanguineous marriage by spontaneous vaginal delivery at a private hospital, with a birth weight of 2500 grams, and cried spontaneously at birth. The mother was a booked case and received regular antenatal care. She did not receive antenatal steroids. The antenatal period was uneventful. The baby had respiratory distress since birth and was kept nil orally on intravenous (IV) fluids, IV antibiotics and oxygen inhalation by head box. The condition of the baby did not improve, and the parents were unable to afford the treatment at the private hospital, so the baby was brought to our hospital at 51 hours of life.
At admission, the baby had a poor activity and hypotonia. Temperature was 99.0° F in the axilla, heart rate was 160/minute and respiratory rate was 116/minute. He had severe sternal, intercostal and subcostal retractions along with cyanosis. The oxygen saturation (SpO2) was 73% on room air and 86% on oxygen by hood at 10 litres/minute. The air entry was bilaterally equal and no added sounds were heard. Examination of the cardiovascular system and abdomen was normal and no congenital anomaly was apparent. On investigations, his hemoglobin was 15.8 g%, with a normal total and differential leucocyte counts. Band cells were not raised in peripheral blood and
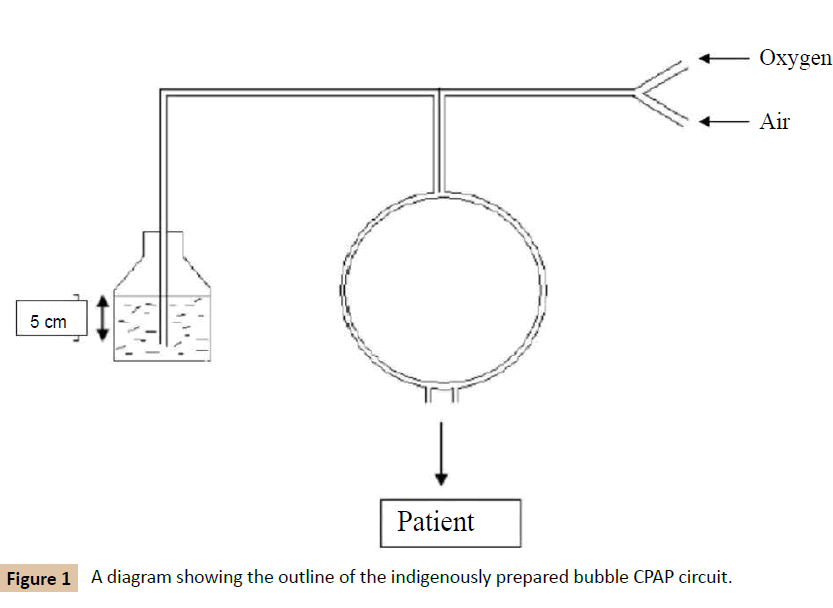
CRP was negative. Chest X-ray at 54 hours of life showed air bronchogram but there was no ground glass appearance of lungs. Blood sugar, urea, serum creatinine and electrolytes were also normal. A blood culture was sent which latter turned out to be sterile. Arterial blood gas estimation was not available at our centre. A diagnosis of RDS was made on clinical grounds. There was no mechanical ventilator or CPAP available in the hospital, so we put the baby on an indigenously prepared bubble CPAP circuit with nasal cannula, with the pressure of 5 cm H2O and FiO2 of 0.6 (Figure 1). For providing CPAP, commercially available nasal prongs were used which were connected to sources of oxygen and compressed air by a three-way connecter. One limb of the nasal prongs was cut and dipped in a 500 ml bottle of normal saline upto the depth of 5 cm. The other cut end of the tube was sealed with a tape to prevent leakage. The baby was kept nil orally, on IV fluids, IV antibiotics (cefotaxime 150 mg/kg/day and amikacin 15 mg/kg/day). He maintained an SpO2 of 95%.
His respiratory distress gradually decreased, FiO2 was gradually brought down to 0.3. After 18 hours, his respiratory rate decreased to 70/minute, and he was maintaining a SpO2 of 98%.
CPAP was removed at this point and he was put on oxygen by hood at 5 liters/minute. By 81 hrs of life, his respiratory distress had settled, and activity and tone improved. Oxygen was removed and he maintained an SpO2 of ≥95% on room air. Breast feeds were started which the baby accepted well. As there was no clinical or laboratory evidence of sepsis, antibiotics were stopped after 72 hours. The baby was discharged on day 5 of life on exclusive breast feeding.
Discussion
The neonatal mortality in India is still amongst the highest in the world. Almost a quarter of the burden of neonatal mortality is shared by India. Of the 26 million babies born annually in our country, 65% are delivered at home and more than half by semiskilled and unskilled Traditional Birth Attendants [1]. Most of the deliveries in our country still take place in ill-equipped centers and facilities for neonatal transport are almost non-existent. Hence, there is a need for low cost methods for providing care to the high risk newborns in peripheral health care Centre’s.
Nasal CPAP is widely used for a variety of neonatal respiratory conditions all over the world. It is established as an effective method of preventing extubation failure, is used in the management of apnoea of prematurity, and is increasingly seen as an alternative to intubation and ventilation for the treatment of RDS [2,3].
In our case, the baby required ventilator support, but our hospital had only two mechanical ventilators and both were occupied at that moment. Hence we prepared an indigenous bubble CPAP circuit to salvage the baby. A diagram of our circuit is shown in Figure 1. The bubble CPAP circuit that we utilized was first described by Kaur et al. [4], which can deliver 21% to 98% of oxygen. We did not have the humidifier, so we provided unhumidified oxygen to the baby.
Furthermore, we could not perform ABG due to unavailability. Nevertheless, with the help of this low cost indigenous method, we were able to salvage this baby, which could probably otherwise have deteriorated.
This case highlights the possibility of wider application of such indigenous techniques in resource poor settings in the developing nations, which may contribute in lowering the neonatal mortality, but further studies on an adequate sample size are required before making any recommendations.
References
- Nair MKC, Jana AK, Niswade AK (2005) Neonatal survival and beyond. Indian Pediatr. 42: 985-988.
- Davis PG, Henderson-Smart DJ (2002) Nasal continuous positive airway pressure immediately after extubation for preventing morbidity in preterm infants. The Cochrane Library, Issue 1. Oxford: Update Software.
- De Paoli AG, Morley C, Davis PG (2003) Nasal CPAP for neonates: what do we know in 2003? Arch Dis Child Fetal Neonatal Ed 2003; 88:F168–F172.
- Kaur C, Sema A, Beri RS, Puliyel JM (2008)A simple circuit to deliver bubbling CPAP. Indian Pediatr. 45: 312-314.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences