Prevalence Study of Molar-Incisor Hypo Mineralisation in Primary School Children in South China
Yong-Long Hong, Haiyan Wu, Jialu Yuan, Hongying Yao and Wen Sui
DOI10.21767/2471-805X.100026
Yong-Long Hong1, Haiyan Wu2, Jialu Yuan2, Hongying Yao2 and Wen Sui1*
1Shenzhen Hospital of Southern University, 1333# Xinhu Rd, Shenzhen, 518000, China
2Children's Hospital of Soochow University, 92# Zhongnan Street, SIP, Suzhou, 215025, China
- *Corresponding Author:
- Wen Sui
Stomatological Center, Shenzhen Hospital
of Southern University, 1333# Xinhu Rd
Shenzhen, 518000, China
Tel: 010-8613625279032
E-mail: wendysui@hotmail.com
Received date: January 24, 2017; Accepted date: February 25, 2017; Published date: February 28, 2017
Citation: Hong YL, Wu H, Yuan J, et al.Prevalence Study of Molar-Incisor Hypo Mineralisation in Primary School Children in South China. J Pediatr Care. 2017, 3:1. doi:10.21767/2471-805X.100026
Abstract
objective: The aim of this study is to investigate the prevalence and putative contributing factors of MIH in primary school students in Suzhou.
Subjects and methods: A total of 1145 primary school students were selected for this study. The MIH prevalence survey and a questionnaire was performed in accordance with the MIH diagnostic criteria enacted by the European Association of Pediatric Dentistry (EAPD). Statistical analysis of the data was performed using SPSS13.0.
Results: The overall prevalence rate was 4.45% with no gender difference. The primary clinical manifestation is demarcated opacities. The highest prevalence occurred in children with two affected molars and two incisors. The problematic teeth were usually symmetrical. MIH occurrence significantly related with whether the children suffered from otitis media and tonsillitis and whether they had used antibiotics in their first three years of life. MIH had no correlation with the children’s family background, feeding methods, and the physical conditions of their mothers during pregnancy.
Conclusion: The MIH prevalence in primary students was 4.45% with mild clinical symptoms. MIH prevalence was correlated with the children’s medical history and use of antibiotics in their first three years.
Keywords
Molar; Incisor; Hypo mineralisation; Prevalence; Contributing factors
Introduction
Molar incisor hypomineralisation (MIH) is a disease of abnormal development of tooth structure, mainly affecting the enamel development of the first permanent molars and often the permanent incisors. The disease was first reported by a Swedish scholar Weerheijim in 1970 [1], followed by scholars from various countries, who named the disease differently. The European Academy of Pediatric Dentistry (EAPD) officially named the disease and established the diagnostic criteria [2]. MIH clinical symptoms vary widely and are generally divided into mild, moderate and severe grades. Mild symptom is characterized by demarcated opacities of white to yellow-brown coloration with clear boundaries. Moderate to severe symptoms include extremely sensitive teeth and post eruptive breakdown. The eruption goes deep from dentin to pulp, even the teeth cannot be preserved. Due to poor enamel mineralization, the enamels are worn and broken down soon after the affected tooth erupts. This will affect dentin or pulp if no immediate treatment is received, resulting in atypical caries development. The disease undergoes rapid progression, and often patients and parents overlook the early symptoms. The affected teeth are very sensitive to air and hot and cold stimuli, in which case the patients are afraid to brush their teeth and see the dentist. The deterioration of the teeth condition, combined with insensitivity of inflamed teeth to anaesthetic, results in substantial challenges to the dentist. Because of the rapid progression and lack of knowledge about the disease, the patients need multiple treatments, thus causing phobia about seeing a dentist and psychological issues among young patients.
Epidemiological studies have shown that there is a great variation of MIH prevalence in different countries, ranging from 4% to 25% [3,4]. This might be due to different diagnostic criteria, statistical methods and children’s physical development. Studies have found that with the decline of dental caries in the western world, MIH prevalence among children is on the rise for unknown reasons [5,6]. No systematic research on MIH has been done in China. The objective of this study is to investigate the prevalence of MIH in Chinese children and the putative contributing factors, through statistical surveys of MIH patient population in primary school students in Suzhou, and further lay the foundation for further studies of the aetiology and treatment of MIH.
Materials and Methods
Subjects
Suzhou is a representative of the southern region of China with a population of approximately 11 million. In 2015, we organized an oral exam screening of MIH on primary school students in Suzhou. A list of the schools and the permission to perform the research at those schools had been obtained from the Department of Hospital Ethical Committee (Date of approval: May, 2015, approval number: 15118). The following cases were excluded: patients with dental fluorosis, enamel hypoplasia, dentin hypoplasia, tetracycline teeth, ongoing orthodontic treatment, periodontal disease, and systemic disease. We randomly selected 1145 primary school students of all grades, with 607 boys and 538 girls. The informed consent was obtained from patients and that the study was performed in accordance with the Declaration of Helsinki.
Diagnostic instrument
Disposable dental instrument package, including the mouth mirror, cotton pliers, and probes.
Examination and diagnosis methods
According to the diagnostic criteria enacted by the European Academy of Pediatric Dentistry (EAPD), all examination for MIH were undertaken on clean wet teeth of the erupted permanent first molars and incisors (Table 1) [7].
| Mild MIH | Demarcated opacities without enamel breakdown. |
| No history of dental hypersensitivity. | |
| No caries associated with the affected enamel. | |
| Incisor involvement is usually mild if present. | |
| Moderate MIH | Atypical restorations can be present. |
| Demarcated opacities are present on occlusal/incisalthird of teeth, enamel breakdown/caries are limited to 1 or 2 surfaces without cuspal involvement. |
|
| Dental sensitivity is generally reported as normal. | |
| Severe MIH | Post-eruptive enamel breakdown is present. |
| A history of dental sensitivity. | |
| Caries is associated with the affected enamel. | |
| Crown destruction can advance to pulpal involvement. | |
| Defective atypical restoration. | |
| Strong aesthetic concerns. |
Table 1: Diagnostic criteria enacted by the European Academy of Pediatric Dentistry (EAPD).
Training of doctors and recording methods
All dentists involved in this study received standardized MIH diagnostic training (criteria by EAPD). Patients who met the MIH criteria were classified as MIH patients. After the oral examination, parents of the participating children were surveyed and recorded.
Statistical analysis
The prevalence of MIH, gender, age, family background, parents’ education level, personal dietary preference, medical history and the use of antibiotics in their first three years were recorded for statistical analysis. SPSS13.0 software package was used for testing the differences between two groups of affected and unaffected children. A probability value of less than 0.05 was considered as significant.
Results
Of 1145 primary school students, 51 were MIH patients. The overall prevalence rate was 4.45%, 4.78% (29 out of 51) in boys and 4.09% (22 out of 51) in girls. There was no statistical difference in gender (P = 0.57). There were 33 MIH patients among 7–8 year olds (prevalence rate is 6.25%), 8 MIH patients among 9–10 year olds (prevalence rate is 2.53%), and 10 MIH patients among 11–12 year olds (prevalence rate is 3.31%). The 7–8 age group had a significantly higher MIH prevalence rate than the other age groups (P = 0.022) (Table 2).
| MIH | NO-MIH | Sum | X2 | P-value | |
|---|---|---|---|---|---|
| Gender | |||||
| Boy | 29 | 578 | 607 | 0.32 | 0.57 |
| Girl | 22 | 516 | 538 | -- | -- |
| Age | |||||
| 07-08 yrs | 33 | 495 | 528 | 7.64 | 0.022 |
| 09-10 yrs | 8 | 307 | 315 | -- | -- |
| 11-12 yrs | 10 | 292 | 302 | -- | -- |
Table 2: The correlation of MIH to gender and age.
MIH prevalence rate was not correlated with the children’s family situation, feeding methods, and the physical conditions of their mothers during pregnancy (P>0.05) (Table 3).
| MIH | NO-MIH | Sum | X2 | P-value | |
|---|---|---|---|---|---|
| Father's education | |||||
| Graduate education | 6 | 181 | 187 | 1.23 | 0.54 |
| Collage | 25 | 550 | 575 | ||
| No Collage | 20 | 363 | 383 | ||
| Mother’s education | |||||
| Graduate education | 3 | 65 | 68 | 15 | 0.93 |
| Collage | 18 | 358 | 376 | ||
| No Collage | 30 | 671 | 701 | ||
| Family income | |||||
| Low | 14 | 215 | 229 | 2.36 | 0.31 |
| Medium | 35 | 851 | 886 | ||
| High | 2 | 28 | 30 | ||
Table 3: The correlation of MIH to family situation.
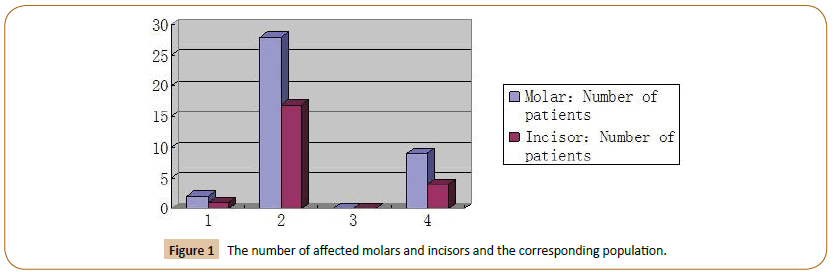
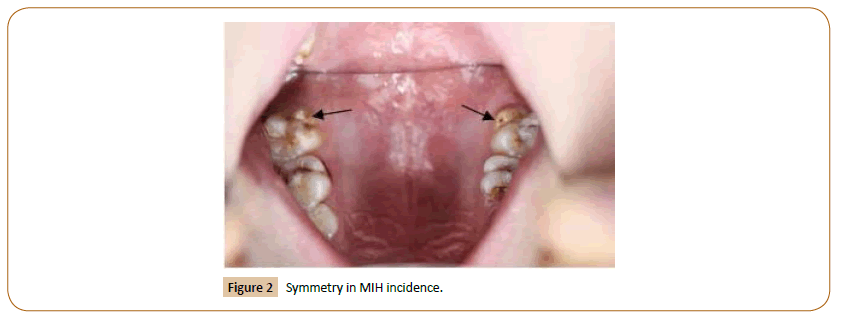
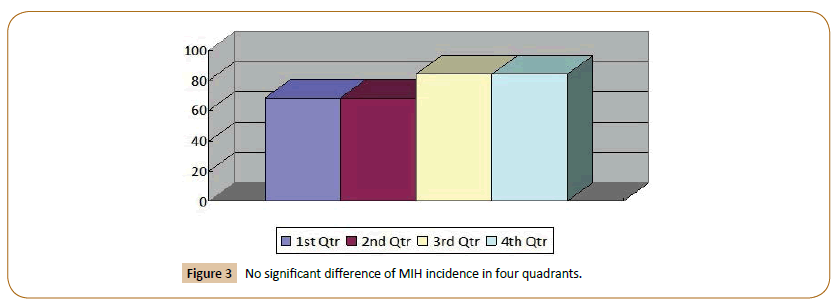
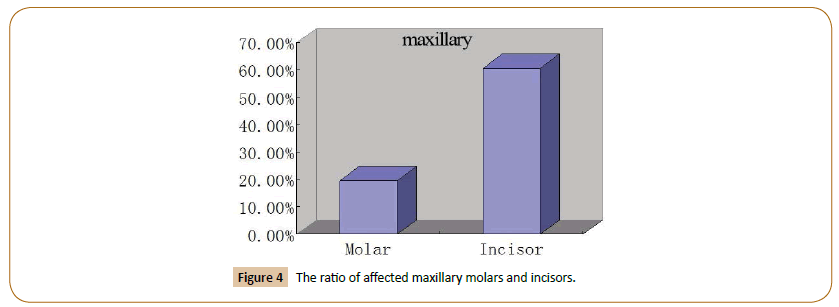
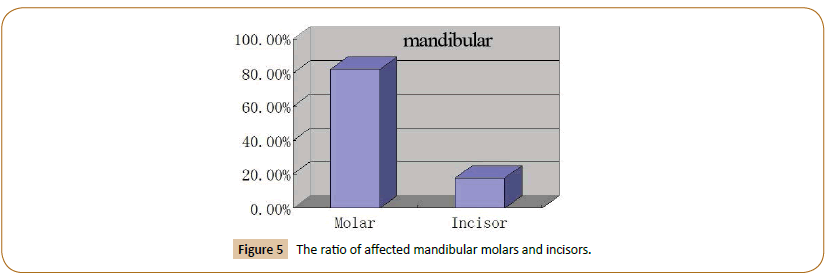
The top three affected incisor numbers in MIH patients were 2, 4, 1. The affected molar numbers in MIH was 2 in most cases, followed by 4 (Figure 1). Odd numbers of affected incisor and molar in MIH patients were less common than even numbers, which suggested the symmetrical nature of MIH symptoms (Figure 2). In most of the cases, 2 molars and 2 incisors were involved in MIH patients (Tables 4 and 5, Figure 1). There was no significant difference in MIH prevalence in the four quadrants of the teeth (Figure 3). In all patients, the prevalence was higher in maxillary incisors than maxillary molars (Figure 4) and the prevalence was higher in mandibular molars than mandibular incisor (Figure 5); there was no significant difference between maxilla and mandible MIH prevalence.
| Affected molar numbers | Patient number (%) |
|---|---|
| 1 | 2 (3.92) |
| 2 | 28 (54.9) |
| 3 | 0 |
| 4 | 9 (17.6) |
| Total | 39 (76.5) |
Table 4: The number of affected molars and corresponding percentage of patients.
| Affected incisor numbers | Patient number (%) |
|---|---|
| 1 | 1 (1.96) |
| 2 | 17 (33.3) |
| 3 | 0 |
| 4 | 4 (7.84) |
| Total | 22 (43.1) |
Table 5: The number of affected incisors and corresponding percentage of patients.
Clinical symptoms
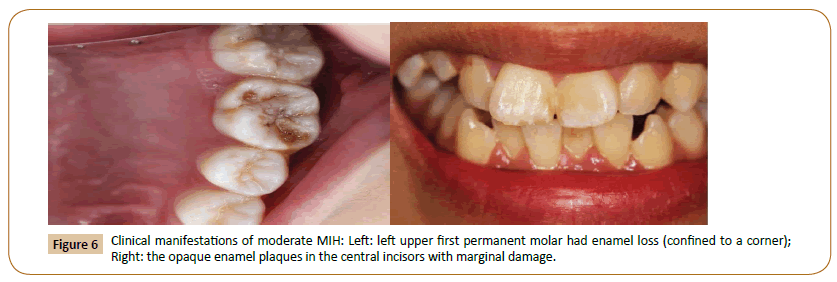
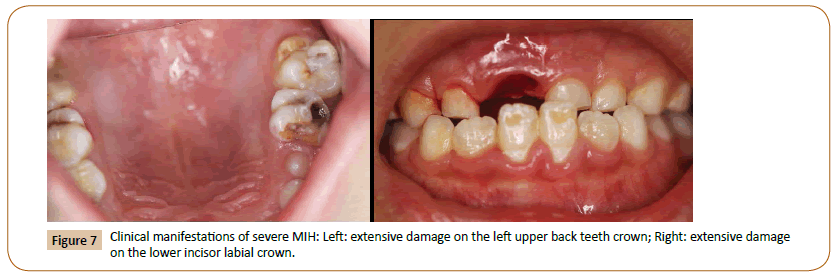
Moderate MIH was seen in 3 molars and 2 incisors (Figure 6). Severe MIH was shown in 2 molars and merely 1 incisor (Figure 7). The rest were mild MIH (Figure 8).
Patients’ health conditions in their first three years, their mothers’ physical condition during pregnancy and feeding methods are shown in Tables 6 and 7. Students with tonsillitis, otitis media and frequent use of antibiotics had a significant higher prevalence of MIH than normal students (P<0.05).
| MIH(%)(N=51) | NO-MIH(N=1094) | X2 | P-value | |
|---|---|---|---|---|
| High fever | 9.8 (5) | 12.0 (131) | 0.22 | 0.64 |
| Tonsillitis | 35.3 (18) | 20 (219) | 6.93 | <0.01 |
| Asthma | 5.9 (3) | 3.8 (42) | 0.13 | 0.72 |
| Otitis media | 11.8 (6) | 4.6 (50) | 3.99 | <0.05 |
| Frequency use of antibiotics | 30 (15) | 0.7 (8) | 189.3 | <0.01 |
| Chicken-pox | 0 | 4.6 (50) | 1.47 | 0.23 |
| Measles | 0 | 0.3 (3) | ||
| No disease | 64.7 (33) | 60.9 (666) | 0.3 | 0.58 |
Table 6: The correlation between MIH and the physical health of children in their first three years.
| MIH (%)(N=51) | No MIH (%)(N=1094) | |
|---|---|---|
| Sick during pregnancy | 0 | 0.46 |
| Medication during pregnancy | 0 | 0 |
| Breastfeeding | 70.59(36) | 55.3 (605) |
| Premature birth | 0 | 1.19 |
| Underweighted baby | 0 | 0.27 |
| Medication during breastfeeding | 0 | 0 |
Table 7: BMW generation Sources.
Discussion
The MIH prevalence rate in primary school students in Suzhou was 4.45%. There was no significant difference with regards to gender. Mittal have shown that the prevalence rate in India is 6.31% [8], 2.8% in Hong Kong Cho [9], 17.6% in Jordan Zawaideh [10], 18.6% in Iraq [11], and 4% to 25% in Europe [3,4]. Regional differences might be correlated with the environment of child’s growth and development, diagnostic criteria, statistical methods, and age. Our study objectives are primary school students in Suzhou. Our sample size was large and represented the MIH prevalence of children throughout Suzhou. Suzhou has a population of 11 million; thus, this study provided a reference for the follow-up MIH prevalence study across China.
Our research showed that MIH prevalence was the highest among 7-8 year old children. This is the age when the first permanent molars and permanent incisors erupt. MIH is characterized by enamel hypo mineralisation, which renders enamel texture softer and fragile. With the increase of age, the chew bite force increases, causing untreated demineralised enamels more prone to be damaged. Often, patients’ teeth become very sensitive, and children are reluctant to brush their teeth, which leads to poor oral hygiene and plaque accumulation and acid accumulation. The condition is further aggravated with the emergence of deep caries or infection to the pulp and apical periodontitis and the clinical manifestation is more like traditional caries or pulpitis, and periapical periodontitis, thereby masking the original causes of hypo mineralisation and clinical manifestations. Therefore, the diagnosis will be inaccurate and the prevalence of MIH in oldaged students is underestimated. That’s why MIH prevalence was the highest among 7–8 year old children in our research.
Among all the MIH patients, we found that mild symptoms were the most common, with the clinical manifestation of demarcated
opacities of white to yellow-brown discoloration with clear boundaries. The colour change of enamel was due to changes in the enamel composition. With the decrease of mineral composition in the enamel, the ratio of protein and water increases, turning the colour of the enamel yellow-brown. Enamel defects in MIH patients are due to hypo mineralisation during enamel development; however, the thickness of the enamel is normal, which is distinct from the clinical manifestation of patients with enamel hypoplasia. With the overall improvement in healthcare, deep caries caused by severe MIH will be treated soon after patients find which leads to a low detection rate of severe MIH. Our study also showed that the affected teeth were symmetrical, i.e., the affected teeth were positioned symmetrically and occurred at the same time. There was no significant difference in the accumulated number of affected teeth in the four quadrants.
It was possible that etiological factors come into play at certain periods during enamel development, therefore affecting teeth that developed at the same period. We found a higher prevalence in maxillary incisors than in maxillary molars, and mandibular molars than mandibular incisors. The finding has great values in clinical targeted diagnosis and prevention of MIH.
In terms of treatment, currently the major treatment for patients with mild MIH is fluoride varnish and Pit and fissure sealant. It is suggested that children use desensitizing toothpaste and fluoride toothpaste and see the dentist on a regular basis. In addition to the above methods, treatment for patients with moderate symptom includes resin restoration to molars. Bleach and micro abrasion can be used on anterior teeth for aesthetic purposes. In addition to the above methods, patients with severe MIH can receive glass ionomer coverage, composite restoration, resin perfusion, veneers, stainless steel crowns and cast restoration. If all these treatments fail, tooth extraction and orthodontic treatment are an alternative.
The aetiology of MIH has long been the focus of research focus; however, there is still no clear answer. Some scholars believe that the aetiology is multifactorial and includes environmental and genetic factors [12]. Jeremias believes that MIH is caused by deregulation of gene expression during enamel development [13]. Pitiphat and Ghanim [14,15] believe that childhood diseases, such as high fever, chicken pox, and tonsillitis, and maternal caesarean section, dystocia, low birth weight contribute to MIH occurrence [14-16]. Some studies link antibiotic use with MIH [17], the use of amoxicillin during the first year of life has been found to increase the risk for MIH in FPMs [18]. An experimental study suggested that a macrolide caused enamel defects in rats. They concluded that a hypo mineralisation zone in incisors was seen after 4 weeks indicating developmental toxicity of the macrolide [19]. We found in our study that students who suffered from otitis media, tonsillitis, and frequently used antibiotics in their first three years of life had significantly higher MIH prevalence than other age groups. The detail reason is unclear. Chawla found that there is a possible association between MIH and combinations of antibiotic use, ear infections, fevers, and other illnesses in the child’s first three years of life [20]. It has been suggested that any factor, which may cause oxygen deficit in active ameloblasts may be responsible for MIH development. First permanent molars are formed during the embryonic stage and start mineralization at birth or shortly after birth. Mineralization of first permanent molars and permanent incisors is not completed until 3–5 years after birth. We found that MIH prevalence was related to medication of the patients before the age of three. It was possible that the disease or antibiotics induced some regulatory factors that affected the mineralization during enamel development. Further in-depth study needs to be done to identify putative factors. Children with problematic first permanent molars and incisors should be monitored closely and active prevention and treatment should be conducted to reduce damage to enamel and loss of teeth.
MIH is a worldwide disease that needs to be addressed. Not enough awareness has been raised by dentists and the public in China. This study investigated the MIH patients in primary school students in Suzhou, discussed the prevalence of MIH children in China, and the putative factors, thus laid the foundation for further aetiology study and shed light on the treatment of MIH.
Conclusion
The overall prevalence of MIH in primary school students in Suzhou was 4.45%, 4.78% in boys and 4.09% in girls, with no significant gender difference. The prevalence rate in 7 to 8 year olds children was 6.25%, which was significantly higher than in other groups. Mild symptoms were most common and were characterized by demarcated opacities of white to yellow-brown discoloration. In most of the cases, two molars and two incisors were affected and they were symmetrically positioned. In patients, whose incisors and molars were affected, the prevalence distribution was not significantly different in the four quadrants of the teeth (P>0.05). The maxillary incisors prevalence was higher than maxillary molars, and the prevalence in mandibular molars was significantly higher than the mandibular incisor. MIH prevalence was significantly correlated with the patients’ medical history and the use of antibiotics in their first three years of life. MIH prevalence rate had no correlation with the children’s family background, the physical conditions of their mothers during pregnancy and the feeding methods.
Acknowledgement
We would like to thank Department of Community Programs, Children's hospital for their immense help and support to conduct this study.
References
- Jasulaityt L, Veerkamp JS, Weerheijm KL (2007) Molar incisor hypomineralization: Review and prevalence data from a study of primary school children in Kaunas. Eur Arch Pediatr Dent 8: 12–21.
- Weerheijm KL, Duggal M, Mejare I (2003) Judgement criteria for Molar-Incisor-Hypomineralisation (MIH) in epidemiologic studies: A summary of the European meeting on MIH held in Athens. Eur Arch Paediatr Dent 3: 110–113.
- Lygidakis NA, Wong F, Jälevik B, Vierrou AM, Alaluusua S, et al. (2010) Best clinical practice guidance for clinicians dealing with children presenting with Molar-Incisor Hyomineralization (MIH): An EAPD Policy Document. Eur Arch Paediatr Dent 11: 75–81.
- WeerheijmKL, Jalevik B, Alaluusu S (2001) Molar incisor hypomineralization. Caries Res 35: 390–391.
- WeerheijmKL, Groen HJ, Beentjes VE (2001) Prevalence of cheese molar in eleven-year-old Dutch children. ASDC J Dent Child 68: 259–262.
- William V, Messer LB, Burrow MF (2006) Molar incisor hypomineralization: Review and recommendations for clinical management. Pediatr Dent 28: 224–232.
- Shubha A, Sapna H (2014) Molar-incisor hypomineralization: Prevalence, severity and clinical characteristics in 8- to 13-year-old children of Udaipur, India. J Indian SocPedodontics Prevent Dent 4: 322–329.
- Mittal NP, Goyal A, Gauba K,Kapur A (2014) Molar incisor hypomineralization: Prevalence and clinical presentation in school children of the northern region of India. Eur Arch Paediatr Dent 15: 11–18.
- Cho SY, Ki Y, Chu V (2008) Molar incisor hypomineralization in HongKong and Chinese children. Int J Paediatr Dent18: 348–352.
- Zawaideh FI, Al-Jundi SH, Al-Jaljoli MH (2011) Molar incisor hypomineralization: Prevalence in Jordanian children and clinical characteristics. Eur Arch Paediatr Dent12: 31–33.
- Ghanim A, Morgan M, Mariño R, Bailey D, Manton D (2011) Molar incisor hypomineralisation: Prevalence and defect characteristics in Iraqi children. Int J Paediatr Dent 21: 413–421.
- Kuhnisch J, Thiering E, Heitmuller D (2013) Genome-wide association study (GWAS) for molar-incisor hypomineralization. Clin Oral Inverst 18: 677–682.
- Jeremias F, Koruyucn M, Kuchler EC (2013) Genes expressed in dental enamel development are associated with molar-incisor hypomineralization. Arch Oral Bio 58: 1434–1442.
- Pitiphat W, Luangchaichaweng S, Pungchanchaikul P, Angwaravong O, Chansamak N (2014) Factors associated with molar incisor hypomineralization in Thai children. Eur J Oral Sci 122: 265–270.
- Ghanim A, Manton D, Bailey D, Marino R, Morgan M (2013) Risk factors in the occurrence of molar incisor hypomineralization amongst a group of Iraqi children. Int J Paediatr Dent 23: 197–206.
- Whatling R, Fearne JM (2008) Molar incisor hypomineralization: A study of aetilolgical factors in a group of UK children. Int J Paediatr Dent 18: 155–162.
- Beentjes VE, Weerheijm KL, Groen HJ (2002) Factors involved in the aetiology of molar-incisor hypomineralisation (MIH) Eur J Paediatr Dent 3: 9–13.
- Phipps KR (2012) No evidence to support the claim that amoxicillin causes molar-incisor hypomineralization. J Evid Based Dent Pract 12: 73–75.
- Abe T, Miyajima H, Okada K (2003) Effects of a macrolide antibiotic on enamel formation in rat incisors--primary lesion of ameloblast at the transition stage. J Vet Med Sci 65: 985–988.
- Chawla N, Messer LB, Silva M (2008) Clinical studies on Molar-incisor hypo mineralization: Distribution and putative associations. Eur Arch Paediatr Dent 9: 180–190.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences