Pediatrics Burn Management Protocol for Nurse Professionals and Students
Berhanu Wale Yirdaw*
Department of Pediatrics and Child Health Nursing, Teda Health Science College, Gondar, Ethiopia
- *Corresponding Author:
- Berhanu Wale Yirdaw
Department of Pediatrics and Child Health Nursing,
Teda Health Science College, Gondar,
Ethiopia,
Tel : 251924526243;
E-mail: berhanuwale7@gmail
Received: February 18, 2022, Manuscript No. IPJPC-22-11913; Editor assigned: February 21, 2022, PreQC No. IPJPC-22-11913 (PQ); Reviewed: March 07, 2022, QC No. IPJPC-22-11913; Revised: March 11, 2022, Manuscript No. IPJPC-22-11913 (R); Published: March 18, 2022, Invoice No. IPJPC-22-11913
Citation: Yirdaw BW (2022) Pediatrics Burn Management Protocol for Nurse Professionals and Students. J Pediatr care Vol:8 No:2
Abstract
Burn is an injury to the skin or other organic tissues caused by a variety of etiologic mechanisms and are common as well devastating in children. In addition to those who die, millions more are left with lifelong visible physical and the invisible psychological scars, disabilities, and disfigurements, often with resulting stigma and rejection. To ensure the optimum post-burn quality of life, nurses should be familiar with subsequent assessment and management of burns. The complexity of the injury and the chronic nature of the sequelae of burns require an integrated multidisciplinary approach with continuous and long follow up, it can lead to the best outcomes. This protocol is prepared from various evidence based articles and up-dated guidelines with the aims to aid and facilitate how nurse’s approach pediatric patients presented with burn injury.
Keywords
Pediatric burn; Prevalence; Disfigurements
Introduction and Epidemiology
A burn is an injury to the skin or other organic tissue caused by a variety of etiologic mechanisms. It is one of the most devastating conditions enocuntered inh ealth care and a significant problem. However, within all countries, burn risks, prevalence and mechanisms vary and correlate with various risk factors like age, sex, and socioeconomic status. It is more significant in low and middle-income countries and even if it affects all ages, children (pediatrics age groups) are particularly vulnerable to burns [1-3].
According to World Health Organization (WHO) estimation, every year 180,000 deaths are caused by burns and out of these children’s accounts, large numbers (although not quantified) and the majority of burn-related deaths occur in low and middleincome countries [2]. The majority of the victims are boys and also more common in younger children [3]. Children under 5 years of age in Africa have over 2 times the incidence of burn deaths than worldwide and account two thirds out of global death. Sub Saharan Africa has the highest number of pediatric burn admissions in the world. As most literature revealed mostly burns occur mainly in the home and workplace [1,2]. In Ethiopia, similar epidemiology and risk factors were reported [4].
In addition to those who die, millions more are left with lifelong visible physical and the invisible psychological scars, disabilities, and disfigurements, often with resulting stigma and rejection [1,2].
Cause and/or mechanism of injury and risk factors
The causes and mechanisms of injury vary with age, sex, and socioeconomic status as well as other risk factors. The extent of a burn injury depends on its cause and mechanism of injury as well as tends to be physiologic change and tissue damage (superficial, deep or full-thickness). The common types of burn injuries are thermal (scald and flame), chemical (acids and alkalis), electrical, and radiation (sunburn). Most of (more than half) of pediatric burns are caused by scald (hot liquid like hot water or coffee), commonly in kitchen and the common mechanism of injury is spilling or exposed by means of abuse [2,3,5].
Electrical injuries; the main determinant of the degree of tissue damage is voltage, it can be low voltage (<1000 volt, mostly household currents 240 volts) or high voltage (>1000 volt). The extent of the injury is mostly cardiac dysrhythmias, but in the case of high voltage injury, there is extensive tissue damage and often limb loss. There is usually a large amount of soft and bony tissue necrosis. Muscle damage gives rise to rhabdomyolysis (the rapid disintegration of skeletal muscle tissue following injury) and renal failure secondary to myoglobinuria may occur [5-7].
Contact: Contact with the hot surface and common sources are curling iron, fireplace glass, oven, space heater, iron, grill, and lamps are also reported [5,8].
Chemical: Result from exposure to either acid or alkali. Acid burns cause coagulation of the skin, which seems to limit the depth of penetration. Alkali burns cause liquefaction and thus result in a deeper injury [5,6,9].
Inhalation: Rresults from direct heat (greater problems with steam burns), CO poisoning and toxic fumes, including from combustible plastics. It is serious if preexisting pulmonary conditions are present. Exposure to smoke may cause degradation of surfactant and decrease its production, resulting in atelectasis [7].
There are so many risk factors for burn including abusers, such as alcoholism, epilepsy or chronic psychiatric or medical illness. All such problems need to be addressed when managing patients in order to speed recovery and prevent a repetition of injury.
Other risk factors for burns, including; occupations that increase exposure to ire, overcrowding and lack of proper safety measures, placement of young girls in household roles such as cooking and care of small children, underlying medical conditions, including peripheral neuropathy, and physical and cognitive disabilities, easy access to chemicals used for assault (such as in acid violence attacks) and use of kerosene as a fuel source for non-electric domestic appliances [1,2].
Estimating percentage of burn size
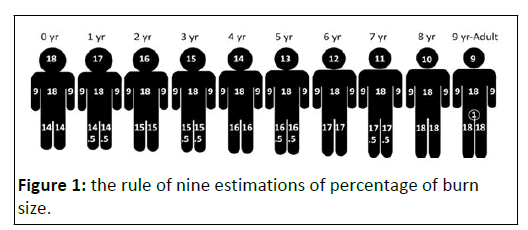
Calculating total body surface area is used to determine the extent of a burn injury and helps for diagnosis, treatment, prognosis, three methods are used; the rule of nine, the Lund- Browder chart and the palm method (Figure 1).
Rule of nine: less accurate and can be used for patients >10 years of age, which divides the body surface into areas of 9% or multiples of 9%, with the exception of the perineum (genitalia) which is estimated at 1% [5,10-12].
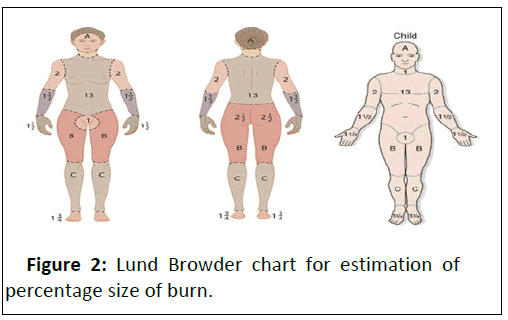
Lund-Browder Chart: more accurate and preferred for pediatric patients (but less accurate for obese children) (Figure 2) (Table 1).
| The relative percentage of area affected the age | |||||
|---|---|---|---|---|---|
| Up to 12 months | 1 years | 5 years | 10 years | 15 years | |
| A; half of head | 9 ½ | 8 ½ | 6 ½ | 5 ½ | 4 ½ |
| B; half of thigh | 2 ¾ | 3 ¼ | 4 | 4 ¼ | 4 ½ |
| C; half of leg | 2 ½ | 2 ½ | 2 ¾ | 3 | 3 ¼ |
Table 1: Lund Browder chart for estimation of percentage size of burn.
Palm method; used for small, irregular or patchy burns over multiple surfaces [6,10,12].
Based on the size of the patient's palm and palmar surface of the hand not including fingers is 0.5% and with fingers is 1% (Figure 3).
It is the least accurate method [5,10,12,13].
Pearls: superficial burns are not included in the total body surface area estimation.
Classification
The presentation and severity of burn injury are determined by the type of burn, duration of contact, the temperature at which the burn occurred, the ability of the contact material to transfer heat, location of the burn wound and the age of the burned patient [8,13].
Based on the mechanism (cause) of injury: Common types of burn injuries are thermal (scald, flame and contact) which occur as the result of heat transfer, specifically through conduction, radiation, or convection, Chemical injury by tissue exposure to noxious substances (acids, alkalis and organic compounds), Electrical due to high voltage, low voltage or lightning strikes, inhalation injury and Radiation (sun-burn) due to exposure to ionizing radiation.
Tissue damage occurs when radiant energy is transferred to the body, stimulating the formation of highly reactive chemicals.
When these chemicals interact with normal body chemicals, they form cellular toxins that target rapidly growing cells. The areas of the body with the most rapidly growing cells involve the skin, GI tract, and bone marrow [11-13].
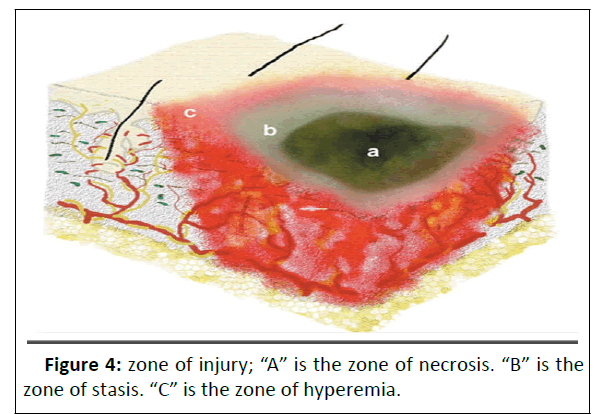
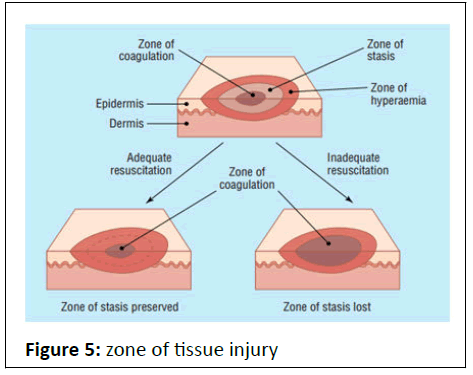
Based on tissue injury: Based on the extent of tissue damage (dependent on; temperature, length of exposure) divided into three; zone of Coagulation, Zone of Stasis and Zone of Hyperemia [5,9,12].
Zone of Coagulation: the center of burn, had the most contact with heat source and point of maximum damage.
The tissue may be non-viable and irreversible due to the coagulation of cells and the denaturing of proteins [5,9,12].
Zone of Stasis: surrounds the coagulation area and characterized by decreased tissue perfusion due to vessel constriction and thrombus formation producing transient ischemia
The tissue is potentially salvageable and the severity of this zone can be minimized by accurate fluid resuscitation [5,9,12].
Zone of Hyperemia: the outermost area of burn injury and characterized by vasodilatation (adequate perfusion due to patent blood vessels) and inflammation, which manifests clinically as an outer zone of erythema due to diapedesis (passage of blood cells) (Figure 4 and 5).
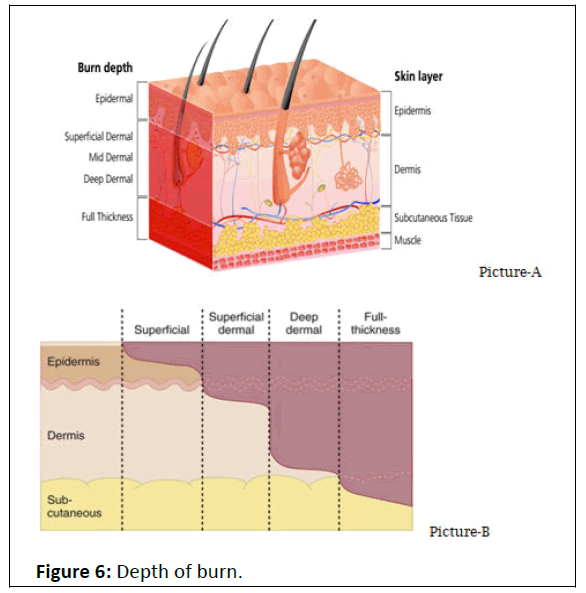
Based on depth
First degree: also called superficial burn and involve only the epidermal layer. Commonly seen resulting from sunburn or minor scalds and the area appears pink or light red and blanches with pressure. The burn is dry, without blister formation and is painful to touch. Typically heals in less than one week without scaring [6,8,10,11].
Second degree: is also known as partial-thickness burns and subdivided into
superficial and deep partial-thickness burns [6,8,11].
A superficial partial-thickness burn: involves the epidermis and the papillary layer of the dermis. They present with blisters and bullae and are typically bright red or mottled in color. They have a moist surface, and the superficial skin can be wiped away. These burns are extremely painful, as the nerve endings are exposed. With proper care, they heal within 7–21 days with a small risk of hypertrophic scarring (the deeper the burn, the slower the healing process and the more of the dermis involved, the more the scarring potential [6,8,10,11].
Deep partial-thickness burns: involves the epidermis and both the papillary and reticular layers of the dermis. Most are caused by flame, oil grease, and very hot liquids. The skin may appear yellow-white (paler) or dark red (non-blanching), with a dry or mildly moist surface. There is a sensation to pressure only, secondary to nerve destruction. These injuries may be difficult to distinguish from third-degree burns and may require >21 days (up to two months) for healing with residual scar formation.
Third-degree or full-thickness burn: usually caused by flame, hot grease or oil, chemicals, or prolonged immersion. All skin elements are lost, with coagulation of blood vessels. The skin is dry, hard, leathery, white (grayish-white), and waxy. Thrombosed superficial veins may be visible. The patient may not have sensation (a little beat has a sensation to deep pressure) because the nerve endings have been destroyed. Wound closure requires resurfacing and grafting because the burned surface will not support the migration of normal epithelium from the unburned periphery [5,6,8,10,11].
Fourth-degree burns: have the same etiologies as thirddegree burns and involve the subcutaneous layer, fascia, tendon, muscle, and/or bone. The extensive amount of necrotic tissue can produce systemic toxicity from tissue breakdown products and deep infection (Figure 6).
Based on the severity of the burn, the involved BSA and the risk groups
Minor burns: First-degree, as well as second-degree injuries encompassing <10% TBSA. And also, partial or full-thickness burns <5% TBSA in a child under ten years of age, partial or fullthickness burns <10% TBSA in a child ten years of age or older, and full-thickness burns <2% TBSA [8,11].
Moderate burns: partial-thickness burns that cover 10-20% TBSA and full-thickness injuries covering <10% TBSA. And also, partial or full-thickness burn involving 5-10% TBSA in a child younger than ten years of age, partial or full-thickness burns involving 10-20% TBSA in a child ten years of age or older, fullthickness burns involving 2-5
TBSA, suspected inhalation injury, a nd circumferential burns are considered as moderate.
Major burns: partial-thickness burns >20% TBSA and thirddegree burns <10% TBSA, as well as burns of the hands, face, eyes, ears, feet, and perineum. Any burn in an infant, any burn involving the face, eyes, ears, genitalia, or joints, burns complicated by fractures or other trauma, high voltage burns, burns complicated by inhalation injury, partial or full-thickness burns of >10% TBSA in a child under ten years of age, partial or full-thickness burns >20% TBSA in a child ten years of age or older, and full-thickness burn >5% TBSA are also included.
Pathophysiology
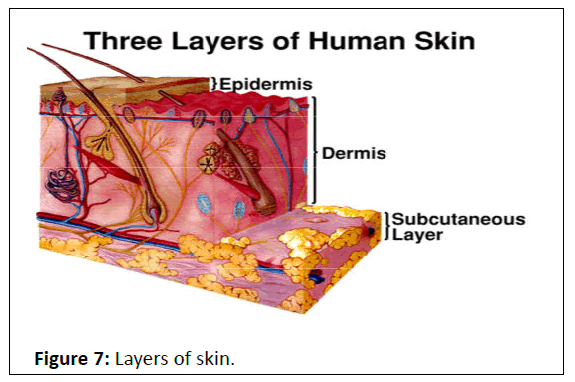
The skin is the largest organ in the body and composed of three layers with its own specific functions. The epidermis is the outer layer and acts as the barrier to infectious agents as well as preventing fluid loss from the body. The second layer is called dermis, which contains the adnexal (accessory structures) e.g., hair follicles, sweat glands, and neural receptors for pain and pressure. It also contains blood vessels, which contribute to the temperature regulation of the body via radiant heat loss. The third layer is called subcutaneous tissue (hypodermis) composed of a fatty layer of skin that contains blood vessels, nerves, lymph, and loose connective tissue filled with fat cells. Therefore children with extensive burns have a loss of these physiologies and difficulty retaining fluid, regulating temperature, and are at risk of infection [6,10] (Figure 7).
Local response; damage to human skin by heat results in two types of injury: an immediate direct cellular response and a delayed response caused by dermal ischemia. Irreversible cellular damage from protein denaturation occurs at temperatures exceeding 45° C. Three zones of injury demonstrate the local pathophysiologic response of tissue damage [8].
Systemic response: release of inflammatory mediators from the damaged cell and tissues (e.g., arachidonic acid metabolites, oxidants, histamine, serotonin, kinins, other vasoactive amines) causes initial vasoconstriction followed by vasodilatation and increased capillary permeability. The increased permeability permits fluids, electrolytes, and plasma proteins to leak into the surrounding tissue (interstitial space), which creates intravascular volume deficits. The release of fluids through the hyper permeable capillaries and the increased capillary pressure combine to create local or systemic edema as well as the potential for severe hypovolemia (leads to burn shock and death) and multisystem organ failure. Sodium, magnesium, calcium, and phosphorus loss can occur directly through open burn wounds. Potassium is released from damaged cells, triggering hyperkalemia and metabolic acidosis [8,12].
The hypermetabolic response post-burn injury is characterized by increased levels of inflammatory mediators, catecholamines, and corticosteroids. The increase in the metabolic rate results in insulin resistance, increased gluconeogenesis, lipolysis, and proteolysis.
Assessment and management
• The complexity of the injury and the chronic nature of the sequelae of burns require an integrated multidisciplinary approach with continuous and long follow up. Only such management can lead to the best outcomes for burn patients [12].
• The main goal of burn care is to ensure optimum oxygenation and resuscitation in the emergency period and then to reach re-epithelialization of injured or destroyed skin and restore the normal physiology of the patient. Subsequent treatment is to ensure the optimum post-burn quality of life. Care for a burned child is divided into three phases; emergent, acute wound care, and rehabilitation [7].
• The emergent phase is the first 72 hours after injury, has a massive capillary leak and burn shock, focusing on thorough assessment and accurate management.
• The acute wound care phase begins when the patient has been stabilized. The goals of this period include healing partial-thickness wounds, grafting full-thickness wounds, and preventing complications.
• Wound management during the acute phase consists of debridement, daily wound care, and surgical interventions for wound closure.
• The rehabilitation phase begins when wound healing is complete and focuses on restoring or maximizing the patient’s functional capacity.
• This phase may last several years and deals with functional and cosmetic problems associated with contractures and scar tissue formation [7].
First aid
• Stop the burn process; remove the patient from the source of burn injury e.g., remove hot, scalding or charred clothing.
• Pearls; avoid self-harm while stopping the burn process.
• Cool the burn wound with cool running tap water (15°C, range 8°C to 25°C) for 20 minutes unless factors (e.g., large burn causing rapid heat loss, hypothermia, and multiple traumas). If it is a chemical burn continue cooling for 1–2 hours (if the chemical is a powder first brush off excess, then irrigate). Keep the remaining areas dry and warm to avoid hypothermia. If the patient’s body temperature falls below 35°C – stop cooling.
• Alert;
• Ice should not be used as it causes vasoconstriction and hypothermia.
• Don’t use grease (e.g., butter, oil) since it predisposes for infection and doesn’t disperse heat.
• If the burn is caused by hot tar, use mineral oil to remove the tar
• Elevate burnt limbs, and head of the bed for burns to head and neck
• Eye burns require flushing adequately i.e. until PH is neutral.
ABCDE principles
Airway with C-spine Protection
• To ensure airway maintenance and provide tissue oxygenation, early recognition of airway compromise followed by prompt intervention should be completed [8,9,13-15].
• Assessment of the airway includes;
• Inspect the airway for foreign material or edema.
• Remove any foreign body (burning agent)
• If not patent, opens the airway with a chin lift and jaw thrust.
• Use airway adjuncts (e.g., oral (guedel) airway and endotracheal intubation.
• Endotracheal tube size and depth; age+4 divided by 4 and 3×ETT size, respectively.
• Use ½ sizes smaller for the cuffed tube.
• Stabilize the neck for suspected cervical spine injury. Keep movement of the cervical spine to a minimum and never hyper-flex or hyperextend the head or neck
• For further reading; Pearls; younger pediatric populations are at high risk due to large tongue/tonsils with the small oral cavity, the narrowest portion of airway, and mild edema can result in airway loss.
Breathing
• Determine if the patient is moving air or not. Assessment of breathing includes;
• Look chest movement
• Listen to breath sounds
• Feel the movement of air through nose or mouth
If breathing compromised;
• Intubate and ventilate the patient with oxygen
• Determining if there are circumferential burns to the chest which may inhibit ventilation.
• Consider carbon monoxide poisoning, central cyanosis and/or non-burnt skin may be cherry pink in color.
• Need to check arterial blood gases (ABGs) and check CO levels
Circulation
Assess perfusion status (circulation and cardiac status) by the following techniques;
• Does the child have warm or cold extremity (hand)?
• Is the capillary refill time ≥ 3 seconds?
• Pulse rate (weak or fast)
• Monitor urinary output
• If any bleeding, stop it.
• Put on oxygen
• Make sure the patient is warm
• Fluid resuscitation
• The goal is to support organ perfusion with the least amount of fluid.
• Indicated for burns of ≥10% of Body Surface Area (BSA), all inhalation burns regardless of TBSA burn and electric burnsto ensure forced alkaline diuresis in case of muscle injury to avoid myoglobinuric renal damage [5,8,9,13-16].
• If possible, IV line should be on the intact skin but access through burned areas may be secured.
• If IV couldn’t be found, use the intraosseous route.
The fluid choice for resuscitation;
• Crystalloid; ringer lactate (the best choice because it has a buffering effect) and 0.9% normal saline.
• Colloid; albumin and blood.
• Due to the capillary leak, not indicated to use colloids within the first 24 hours.
• If used in the early phase (up to 12 h), it can lead to prolonged tissue edema and consecutive lung complications.
• But if the burn is >85% of TBSA can replace colloidconcurrently (early period)[6,7].
Dose and administration;
• For children with severe burn (≥ 20% TBSA) and/or shock, give 20 ml per kg bolus of crystalloids (lactated Ringer’s solution or normal saline) until the assessment of the extent of the burns and calculation of the rest of the fluid of the 24 hours is completed.
• Also consider dopamine (5–20 mcg/kg/min) if poor perfusion persists [6,11,17]. Patients not in shock; treat based on parkland formula;
• 4 ml * %TBSA * weight plus maintenance fluid.
• Half of the fluid is given in the first 8 hours of the resuscitation, calculated from the time of onset of burn injury and the remaining half over the next 16 hours.
• When calculating the initial fluid requirements, it is important to subtract the bolus fluids given from this amount.
• Children younger than 5 years of age require the addition of 5% dextrose in the first 24 hour of resuscitation.
• For the second 24 hour, patients will begin to reabsorb edema fluid and to diuresis. One half of the first day's fluid requirement is infused as lactated Ringer solution in 5% dextrose.
• To determine maintenance fluid use 4/2/1 rue for one hour or 100/50/20 rule for 24 hours.
• 10 ml * first 10 kg plus 4 ml * the second 10 kg plus 2 ml * the remaining kg or
• 100 ml * first 10 kg plus 50 ml * the second 10 kg plus 20 ml * the remaining kg.
Pearls;
• Shock is common in children with burns that involve more than 10% to 12% of the total body surface area.
• Don’t put adhesive plaster circumferentially to the body as it can cause circulatory insufficiency
Monitoring while on fluid;
• The adequacy of resuscitation should be constantly assessed by means of vital signs as well as urine output, blood gas, hematocrit, and serum protein measurements [6,7,14,18,19].
• Urinary catheterization to urine output and hydration status.
• Target urine output (adolescents; 0.5 -1.0 ml/kg/hour, child; 1 ml/kg/hour and infant; 2 ml/kg/hour).
• If urine output less than the target output, increase IV fluids by 1/3 of the current IV fluid amount.
• If urine output greater than target urine output, decrease IV fluids by 1/3 of the current IV fluid amount.
• Additional fluids may be required in severe electrical burns causing muscle damage, as myoglobin may cause renal failure secondary to renal tubular deposition, and therefore maintaining adequate glomerular filtration is very important.
• Check the urine (with a dipstick) for hemoglobin or myoglobin; if positive, obtain a microscopic urinalysis to differentiate hematuria from rhabdomyolysis. If myoglobin is present, increase the fluid rate to maintain a brisk urine output (2 ml/kg/hour) and also consider the administration of sodium bicarbonate to raise urine PH.
• Avoid Over-resuscitation, which causes fluid creep (extremity/ orbital edema, abdominal compartment syndrome, pulmonary edema, cerebral edema) and Under Resuscitation, which causes hypovolemia, shock and organ failure (Kidney failure).
Colloids;
• Albumin (5%); to maintain the serum albumin levels at the desired level (2 g/dl) transfuse with the following rates over 24 hours;
• For burns of 30–50% of TBSA, 0.3 ml of 5% albumin/kg/% TBSA
• For burns of 50–70% of TBSA, 0.4 ml/kg/% TBSA
• For burns of 70–100% of TBSA, 0.5 ml/kg/% TBSA
• Pearls; plasma proteins are important in maintaining oncotic pressure to balance the outward hydrostatic pressure [5,13,19-21].
• Blood transfusion (packed red blood cells); if the hematocrit falls to <24% (hemoglobin=8 g/dL).
• Patients with systemic infection, hemoglobinopathy, cardiopulmonary disease, anticipated (or ongoing) blood loss, and if repeated excision and grafting of full-thickness burns having hematocrit <30% or hemoglobin <10 g/dl also needs a transfusion.
Disability
• Detect if there are any manifestations of neurological deficits
• Impaired on Glasgow coma scale or not
• Establish a level of consciousness
• A – Alert
• V – Response to Vocal Stimuli
• P – Response to Painful Stimuli
• U – Unresponsive
• Examine the pupillary response to light.
• The response should be brisk and equal.
Pearls;
• When treating a burned extremity, vascular assessment is imperative [7,16].
• Be creative in the application of a dressing to this area so that the nurse should check pulses and sensory functions regularly without doing a complete dressing change [7,14,19,22]
Exposure
• Fully assess burn area and depth
• Full examination for concomitant injury
• Keep warm
Admission criteria
• Partial-thickness burns >20% BSA
• Full-thickness burns >5–10% BSA
• Smoke inhalation associated burn
• High voltage electrical burn
• Third-degree burn
• Circumferential burn
• First or second-degree burn to hands, feet, face, perineum, or joints
• Burns <20% BSA and other concerns, e.g. age <12 months, parents not coping, etc.
• Suspected child abuse or neglect
• Comorbiditiesthat may complicate the acute recovery phase
• Other significant injuries like fracture
Supportive
Pain Management
First degree burn
• Acetaminophen (10–15 mg/kg q 4 hour) or ibuprofen (10 mg/kg q 6 hour).
• Hydrocortisone ointment (1%) may help reduce the pain and swelling of severe sunburn, especially if the eyelids and face are involved, but do not apply steroids to higher-degree burns because they increase the risk of infection [6,7,9,13,14,16].
• Severe itching can occur after a few days and persist for more than one week; treat with diphenhydramine (5 mg/kg/day qid, a maximum of 50 mg/dose).
Second, third and fourth-degree burn;
• Analgesics; intravenous analgesics is preferable than IM injections or PO doses because with significant burns circulation to muscle and gut is reduced, and absorption of medication erratic, additionally, intramuscular injections are painful.
• Opioids remain top choice for severe burns
• For instance; fentanyl (1.5 mcg/kg)
• Morphine sulfate
• Oral; 0.3-0.6 mg/kg every 4-6 hour
• IV; 0.05-0.1 mg/kg (maximum, 2-5 mg) every 2 hour.
• Rectal suppositories; 0.3-0.6 mg/kg every 4 hour when oral administration is not possible
For further reading;
Immunization; review child immunization status.
• Burns <10% BSA do not require tetanus prevention.
• Burns >10% need tetanus immunization
• For children <7 years of age, DTaP (If DT, the pertussis vaccine is contraindicated) is preferred to tetanus toxoid alone [5,7,11,15].
• For children ≥ 7 years old and adults, Td preferred to tetanus toxoid alone; DTaP may be preferred if the patient has not previously been vaccinated with DTaP
• TAT; intramuscularly after testing for hypersensitivity
• Dose; Newborn-750 U, Toddlers-1500 U, and Older Children-3000 U)
Nutrition
• The provision of adequate and early nutrition support with the correct balance of nutrients is essential to mitigating the hypermetabolic and hypercatabolic response [7,14].
• High protein diet like milk, meat, egg…etc.
• Sepsis increases metabolic rates, and early enteral nutrition, initially with high-carbohydrate, high-protein caloric support (1,800 kcal/m/24 hour maintenance plus 2,200 kcal/m of burn/24 hour) reduces metabolic stress.
• Calories are provided at approximately 1.5 to 1.7 times thebasal metabolic rate, with 2-4 g/kg of protein/day.
Multi-Vitamins are also necessary;
• Vitamin A; wound healing and tissue repair
• Vitamin B; collagen formation and energy metabolism
• Vitamin C; wound healing, immune system maintenance, antioxidant
• Vitamin D; immunity, metabolism of calcium and glucose
• Vitamin E; protects lipid membranes and antioxidant
• Vitamin K; clotting and bone metabolism
• Zinc; antioxidant, collagen/protein/DNA synthesis.
Wound Care
• The goal is to minimize bacterial colonization and prevent infection
• Debride loose skin and unroof blisters
• Gently clean the burned surface with chlorhexidine solution and rinse thoroughly.
• Topical agents for wound care; with 0.5% silver nitrate solution,silver sulfadiazine cream, nitrofurantoin, mafenide acetate (sulfamylon) cream [5,7,12-14,16,19,23].
• Do not use silver sulfadiazine on the face, for children with hypersensitivity to sulfonamides, or for infants under two months of age (bacitracin ointment is an acceptable alternative).
• Silver nitrate solution causes sodium and potassium loss, need to consider sodium supplementation (oral sodium chloride supplement of 4 g/m burn area/24 hr is usually well-tolerated, divided into 4-6 equal doses to avoid osmotic diarrhea.
• IV potassium supplementation
• If there is evidence of local infection (pus, foul odor), treat with oral amoxicillin (15 mg/kg orally three times a day) and cloxacillin (25 mg/kg orally four times a day).
• If septicemia is suspected, use gentamicin (7.5 mg/kg IM or IV once a day) plus cloxacillin (25–50 mg/kg IM or IV four times a day).
• Honey; has antibacterial and anti-inflammatory properties that may promote healing.
• Proper wound care
• Prophylaxis (penicillin); standard-dose (50, 000 IU/kg) is given orally or intravenously in 4 divided doses for 5 days (5,7,11-14,16).
• Erythromycin may be used as an alternative in penicillinallergic children • Periodic replacement of central venous catheters every 48-72 hr to prevent infection.
Complication
• An infection like bacterial wound infection, pneumonia, urinary tract infection, meningitis if poor wound care and no prophylaxis (5,7).
• Scar and keloid
• Posttraumatic stress disorder
• Organ failure
• Anemia
• Compartment syndrome
• Immune function depression
• Elevated catecholamines, decreased bowel perfusion, and increased gastric secretions place the burn patient at risk for paralytic ileus, intestinal mucosal atrophy, decreased nutrient absorption, Curling stress ulcer, and impaired ability to function as a bacterial barrier
Prevention counseling
• Do not let cooking appliance electric cords hanging off a counter.
• Do not leave hot beverages or foods unattended or near the edge of a table where a child can reach them.
• Keep hot beverages away from children and do not have a child sit in your lap while you drink a hot beverage.
• Teach older children how to safely remove hot food from a microwave or stovetop.
• When carrying hot beverages and foods in the kitchen, ensure children are not in the path of movement.
• Avoid leaving unattended pots on a stove.
• Keep children away from fireplace and wood stove doors with appropriate guards.
• Minimize the storage of flammable liquids and keep them away from areas where children can play and away from any ignition sources.
• Keep matches and lighters where they will not be available to children.
Acknowledgment
Above all, I would like to express my gratitude to our Lord Jesus Christ and his mother the virgin St. marry who carries all my burdens and shepherded my health.
Secondly, my deepest appreciation goes to Mr. Chalachew Adunga, to his valuable support and comment as well as effort. I really appreciate your commitment and assistance; I sincerely thank you so much.
References
- Albertyn R, Numanoglu A, Rode H (2014) Pediatric burn care in sub-Saharan Africa. Afr J Trauma 3:61
- Organization WH. Burn, key fact sheets 201
- Santiso L, Tapking C, Lee JO, Zapata-Sirvent R, Pittelli CA, et al. (2019) The epidemiology of burns in children in Guatemala: a single center report. J Burn Care Res 41:248-253
- Kidanu M, Amdesilasie F, Kassa A, Tadelle Y, Befekadu M (2019) Patterns of Burn Injuries in Ayder Comprehensive Specialized Hospital: a 5-year Retrospective Study, Mekelle, Ethiopia. Afr J Health Sci 1:17-27
- Lisa Wedel APRN CP (2019) Comprehensive Management of Inpatient Burns: A Team Approach. New Orleans
- Cameron P, Browne GJ, Mitra B, Dalziel S, Craig S (2018) Textbook of paediatric emergency medicine: Elsevier Health Sciences
- Robert m, st geme k (2019) Nelson textbook of pediatrics, 21th edition.: elsevier-health Science
- Hockenberry MJ, Wilson D (2015) Wong's nursing care of infants and children-E-book: Elsevier Health Sciences
- Paul VK, Bagga A (2018) Ghai Essential Pediatrics: CBS Publishers & Distributors
- Ganti L, Kaufman MS (2018) First Aid for the Pediatrics Clerkship: McGraw Hill Professional
- Gershel JC, Crain EF (2018) Clinical Manual of Emergency Pediatrics: Cambridge University Press
- Nix D, Bryant RA, Nix DP (2016) Acute & Chronic Wounds: Current Management Concepts: Elsevier Mosby
- Kline MW, Blaney SM, Giardino AP, Orange JS, Penny DJ, et al. (2018) Rudolph's Pediatrics: McGraw Hill Professional
- Federal Democratic Republic of Ethiopia MoH (2014) Emergency Triage Assessment and Treatment
- Melborune Trcsh (2019) Clinical Practice Guidelines, Burns/management of burn wounds
- Sons JW (2016) Advanced paediatric life support: a practical approach to emergencies: John Wiley & Sons
- Crisp S, Rainbow J (2013) Emergencies in paediatrics and neonatology: OUP Oxford
- Mehta M, Tudor GJ (2019) Parkland Formula. StatPearls
- Romanowski KS, Palmieri TL (2017) Pediatric burn resuscitation: past, present, and future. Burns & trauma 5:26
[Crossref][Googlescholar ][Pubmed]
- Paratz JD, Stockton K, Paratz ED, Blot S, Muller M, et al. (2014) Burn resuscitation—hourly urine output versus alternative endpoints: a systematic review. Shock; 42:295-306
- Saffle JR (2016) Fluid creep and over-resuscitation. Critical care clinics 32:587-598
- Cartotto R, Greenhalgh D (2016) Colloids in acute burn resuscitation. Critical care clinics 32:507-523
- Rizzo JA, Rowan MP, Driscoll IR, Chung KK, Friedman BC, et al. (2016) Vitamin C in burn resuscitation. Critical care clinics 32:539-546
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences