Diagnostic Values of Inflammatory Markers at Pediatric Intensive Care Unit
Sofijanova Aspazija*, Bojadzieva Sonja, Shuperliska Elizabeta and Jordanova Olivera
Sofijanova Aspazija*, Bojadzieva Sonja, Shuperliska Elizabeta and Jordanova Olivera
Department of Paediatrics, University Children’s Hospital, Skopje, Republic of North Macedonia
- *Corresponding Author:
- Sofijanova Aspazija
Department of Paediatrics,
University Children’s Hospital,
Skopje, Republic of North Macedonia,
E-mail: aspaziculi@yahoo.com
Received Date: August 25, 2020;Accepted Date: September 10, 2020;Published Date: September 17, 2020
Citation: Aspazija S, Sonja B, Elizabeta S, Olivera J (2020) Diagnostic Values of Inflammatory Markers at Pediatric Intensive Care Unit. Pedfiaftrfic Care Voffl.6 No.4: 3 DOI: 10.36648.2471-805X.6.4.3
Abstract
Background: Sepsis is a major cause of mortality and morbidity in newborns. Early diagnosis and timely use of antibiotic therapy is essential for life-threatening condition, at the Pediatric Intensive Care Unit (PICU).
Objective: The aim of this study is to determinate the values of procalcitonin (PCT) on the outcome of newborns in PICU and find out if these biomarker can be used to predict sepsis.
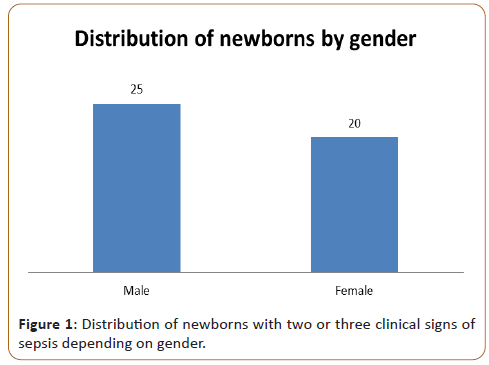
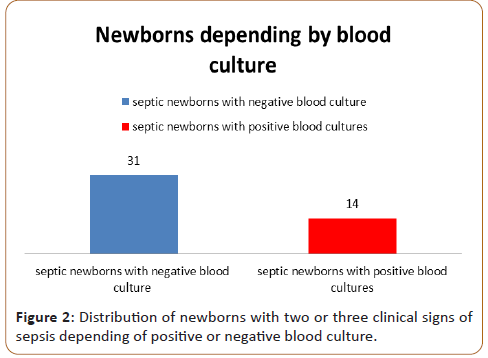
Methods: The study was designed as a retrospective clinical, epidemiological investigation in the period sixth months. We included 45 (M:F=25:20) newborns with two or three clinical signs of sepsis hospitalized in the PICU at the University Children’ Hospital-Skopje. The newborns have been divided into two groups: First group included 31 septic newborns with negative blood culture and second group included 14 septic newborns with positive blood cultures. A sample for blood culture, white blood cells (WBC), C-reactive protein (CRP) and PCT were taken during the first 24 hours of sign of infection, a second sample for 3-5 days, and third sample of 6-14 days. Procalcitonin was determined by immunoassay: patented ELFA (Enzyme-linked fluorescent assay) technology, automated Vidas Biomerieux immunoassay (ng/ml). CRP levels were determined by using immunoturbidimetric method Architect c4000 Abbott (mg/L). White blood cells (WBCs) were determined by using Flow citometry method on Sysmex xs 800i/1000i. The new multiplex polymerase chain reaction-based rapid diagnostic test (BioFire Film Aray Blood Culture Identification) was used for determinate blood culture.
Results: Procalcitonin PCT levels at first 24 hours of the admission were increased in all 45 newborns (≥ 2ng/mL). The values of C-reactive protein gradually increase after 12- 36 hours at admission. The values of WBC increased at 31 new borns, except in 14 new borns with severe sepsis the WBC were decreased (WBC counts<4000). The second measurement, after 3-5 days usage of an adequate antibiotic treatment, the levels of PCT were decreased, except in five new borns severe sepsis were developed, and three patients were developed septic shock. At the third measurement on 6-14 days the levels of PCT and CRP were decreased.
Conclusion: The values of inflammatory markers for sepsis are important clinical significance in predicting the prognosis of newborns with positive and negative blood cultures. Procalcitonin values are most important diagnostic and early prognostic factor for sepsis in newborns, whose values can prevent the development of severe sepsis and septic shock. It is a reliable biomarker whether an appropriate antibiotic for the treatment is used, thus increasing newborns safety, reducing costs and decreased the development of antibiotic resistance. Treatment could be surgical or non-surgical, but specialist expertise is of key importance.
Keywords
Sepsis; C-reactive protein; Procalcitonin; White blood cells (WBC)
Introduction
Sepsis is a major cause of mortality and morbidity in newborns. Early detection of this disease is required in order to initiate therapy in a timely manner and reduce the mortality rate [1]. Neonatal sepsis is the systemic response to infection by microbial organisms, with the highest incidence occurring among newborns of very low birth weight and gestation [2]. Without timely treatment, sepsis can rapidly lead to tissue damage, organ failure, and death in newborns. Preterm newborns are at higher risk for sepsis than term newborns, as they tend to require more invasive procedures than term newborns [3]. Using biomarkers is important assessment for developing sepsis, severe sepsis or septic shock. Unfortunately, the leading factor in morbidity and mortality in the postnatal period is still bacterial inflammation [4]. Newborns with clear signs of sepsis present with features of infection and clinical manifestations of inflammation. Severe sepsis is the development of hypoperfusion with organic dysfunction in a septic newborns. Septic shock is the hypoperfusion with multiorgan failure and persistent hypotension [5,6]. Mortality varies up to 16% in newborns with sepsis and 40%-60% in newborns with septic shock. The research of new biomarkers enabling a precocious identification of newborns at risk of diseases, allowing a close monitoring of the disease and providing information about prognosis, represents a strategic objective of several current researches [7].
Diagnosis of infection caused by bacteria or other microbiological organisms is essential for effective treatment and prognostic evaluation. Current clinical and laboratory methods for diagnosing bacterial infections are either nonspecific or require a longer time to develop the agent. The values of inflammatory biomarkers are important clinical significance in predicting the prognosis of newborns with sepsis and can be used to diagnose bacterial infections. One specific and early biomarker for predicting sepsis is procalcitonin.
Procalcitonin is a peptide precursor to the hormone calcitonin, the latter being involved with calcium homeostasis. It is usually synthesized in the C cells of the thyroid gland and neuroendocrine cells of the lung and the intestine. It occurs when preprocalcitonin is broken down intracellularly under the action of proteolytic enzymes into the active hormone [8]. In structure it is a protein made up of 116 amino acids with a molecular weight of 13 kDa [9]. Procalcitonin has a half-life of 22 to 26 hours and can be detected within 4 hours. The peak occurs between 12-48 hours. Under normal physiological conditions in humans, procalcitonin levels are <0.5 ng/ml. In addition to thyroid cells, PCT is synthesized in other extrathyroid tissues and its concentration can be increased up to 100,000 times in bacterial infection as well as in systemic inflammatory response syndrome. PCT synthesis is activated by a number of pro-inflammatory cytokines released in the presence of bacterial toxins, leading to an increase in PCT concentration. However, the values of procalcitonin can be elevated in diseases other than sepsis, such as autoimmune diseases, heart attack, pancreatitis, trauma, burns, and surgery. Also, many studies have shown that in the early stages, procalcitonin values are higher in chronic diseases such as congestive heart failure and chronic kidney disease, and this should be taken into account when making a clinical assessment using this biomarker [10]. In septic conditions, the value of procalcitonin may be far higher and procalcitonin is more specific in bacterial infections than other acute phase reactants. PCT in clinical practice is used as a biomarker to distinguish bacterial from viral sepsis, as well as non-infectious systemic inflammatory response syndrome [11].
Materials and Methods
The study was designed as a retrospective clinical, epidemiological investigation in the period sixth months. We included 45 (M:F=25:20) newborns with two or three clinical signs of sepsis hospitalized in the PICU at the University Children Hospital- Skopje.
In newborns was diagnosed sepsis according to the standard protocols for disease diagnosis. The clinical criteria taken as indicative of sepsis in newborns was: apnea, tachypnea, respiratory distress,bradycardia, seizures, poor perfusion, lethargy, feeding intolerance, temperature instability, low birth weight, gestational age, gender, and preterm newborns.
All the laboratory examination were analysed in the Clinical Laboratory at the PHI University Children’s Hospital-Skopje. A sample for blood culture, PCT CRP and WBC, the first sample was taken during the first 24 hours of sign of infection, a second sample for 3-5 days, and third sample of 6-14 days.
Blood culture media were incubated at 37°C for 5 days in Bact Alert 3D 360. Positive blood culture was proven with the new multiplex polymerase chain reaction-based rapid diagnostic test (BioFire FilmAray Blood Culture Identification).
Procalcitonin was determined by immunoassay: patented ELFA (Enzyme-linked fluorescent assay) technology, automated Vidas Biomerieux immunoassay (ng/ml) CRP levels were determined by using immunoturbidimetric method Architect c4000 Abbott (mg/L). White blood cells (WBCs) were determined by using Flow citometry method on Sysmex xs 800i/1000i.
Statistical Analysis
The SPSS program was used for statistical analysis, to compare the means of the variables, one-way ANOVA test. Categorical variables between groups were analyzed using the Chi-square test. The results were presented as percentage (%), mean, standard deviation (SD), median, and minimum-maximum (min- max). A p-value<0.05 was considered as significant.
Results
The study was designed as a retrospective clinical, epidemiological investigation in the period sixth months. We included 45 (M:F=25:20) newborns with two or three clinical signs of sepsis hospitalized in the PICU at the University Children’ Hospital- Skopje (Figure 1).
The patient have been divided into two groups: First group included 31 septic newborns with negative blood culture and second group-14 septic newborns with positive blood cultures (Figure 2).
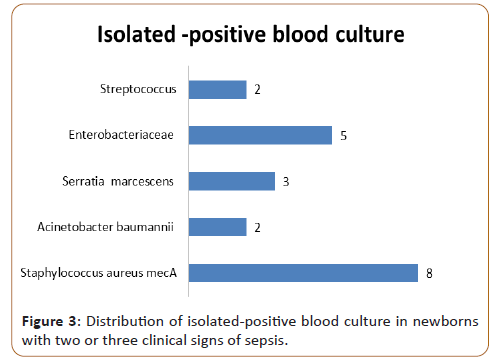
We isolated 14 positive blood cultures who had two or three bacteria at the same time. The identified bacteria included Staphylococcus aureus mecA (n=8), Acinetobacter baumannii (n=2), Serratia marcescens (n=3) Enterobacteriaceae (n=5) and Streptococcus (n=2) (Figure 3).
The mean gestational age of newborns with negative blood culture was 37.39 ± 3.2 weeks and with positive blood cultures 36.36 ± 3.1 weeks. The mean birth weight of newborns with negative blood culture was 2891.7 ± 751.3 grams, while with positive blood cultures was 2675.7 ± 879.1 grams.
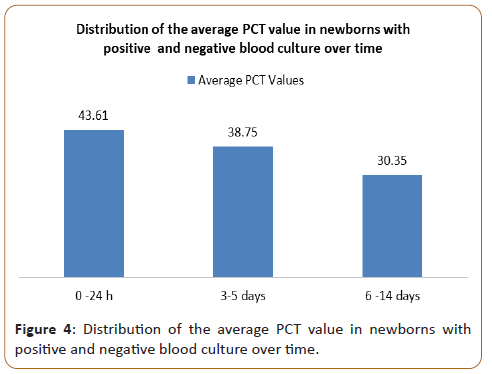
Statistical analysis of correlation of positive and negative blood culture confirmed significantly different values of PCT in the analyzed time period. ANOVA test show statistical significance p<0.001 (Figure 4).
The highest average values (43.61 ± 52.49) were measured in newborns with positive blood culture during admission, with a subsequent sharp jump compared to newborns with negative blood culture. After the second measurement at day 3-5, the average values of PCT in newborns with positive blood culture slowly decreased (38.75 ± 47.25), so that after the third measurement on day 6-14 in newborns with positive blood culture, they slowly decreased (30.35 ± 31.11).
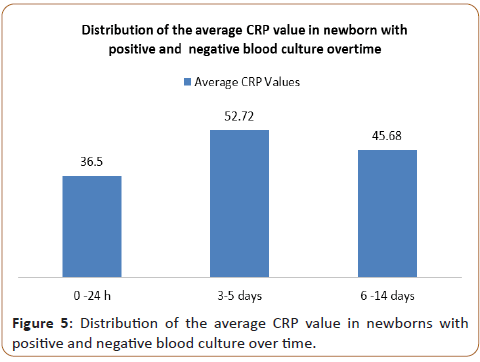
Statistical analysis of correlation of positive and negative blood culture confirmed significantly different values of CRP in the analyzed time period. ANOVA test show statistical significance p<0.001 (Figure 5). At the first measurement, the average values of CRP in newborns with positive blood culture slowly increased (36.67 ± 50.43). The highest average values in newborns with positive blood culture were measured (52.72 ± 85.69) after the second measurement on day 3-5, with a subsequent sharp jump compared with newborns with negative blood culture. At the third measurement in newborns with positive blood culture on day 6-14, the average values of CRP slowly decreased (45.68 ± 72.52).
In our study we confirmed that there is no correlation between values of WBC in newborns with sepsis with positive and negative blood culture in the analyzed time period. The average levels of three measurement (14.62 ± 8.26, 15.71 ± 9.64. 14.61 ± 12.61) there is no statistical significance p>0,05.
In the three measurements, at the 14 newborns with severe sepsis and septic shock we confirmed very decreased value of WBC (3.72 ± 5.26, 3.78 ± 5.64. 3.81 ± 9.71).
Average serum albumin values in newborns with positive blood cultures showed lower values compared with the newborns with negative blood cultures (25,22 ± 2,6 g/L versus 31.81 ± 5,1 g/L).
Average total serum protein values in newborns with positive blood cultures showed lower values compared with the newborns with negative blood cultures (45,01 ± 5,2 g/L versus 50.51 ± 6,1 g/L).
Hypoxia was reported in 25/45 newborns with positive blood cultures and 25/45 full-term newborns with negative blood cultures, with mean partial pressure values оf O2 5,22 ± 0,8 KPa versus O2 5,35 ± 1,2 KPa.
Hypercapnia was reported in 20/45 newborns with positive blood cultures and 29/45 newborns with negative blood cultures.
Capillary blood test findings show lower mean pH in newborns with positive blood cultures compared with newborns with negative blood cultures (7,18 ± 0,14 versus 7,23 ± 0,12).
Discussion
Pediatric sepsis is a life-threatening condition which consists a range of disorders, leads to damage tissues and organs [11]. Early recognition and treatment clearly improves the outcome of newborns with infection leading to sepsis.
In our study, we examined three parameters PCT, CRP, and WBC in newborns with two or three clinical signs of sepsis.
One promising biomarker has been procalcitonin (PCT), whose concentration has been found to be elevated in sepsis [12,13]. Many authors found that procalcitonin is a promising marker for the diagnosis of sepsis in newborns [14]. An ideal biomarker for sepsis should have high sensitivity and specificity, with early phase of diagnostic, low cost and quick result. Procalcitonin has a clinical setting in the following situations: differentiation of bacterial from viral infection; diagnosis of sepsis and septic shock as well as monitoring of this condition and stratification of the risk; determining the length of antibiotic treatment; monitoring the response to antibiotic therapy; diagnosis of bacteremia and sepsis in children including neonates; diagnosis of secondary systemic infection and diagnosis of bacteremia in patients with neutropenia [15,16].
Our statistical analysis of correlation of positive and negative blood culture confirmed significantly different values of PCT in the analyzed time period. ANOVA test show statistical significance p<0.001 (Figure 4). The highest average values (43.61 ± 52.49) were measured in newborns with positive blood culture during admission, with a subsequent sharp jump compared to newborns with negative blood culture.
If procalcitonin levels do not fall or increase, it is a negative prognostic indicator of infection control or response of the host to antibiotic therapy. In this case, additional diagnostic tests are needed and broad-spectrum antibiotic therapy is start [17- 19]. Based on all this data, in a patient with a clinical picture of sepsis or septic shock, the initial level of procalcitonin should be checked, and then the next check of the level of this biochemical marker should be in two days [20]. The results of our study are in correlation with data from the literature [21-23].The diagnostic performance of PCT in numerous studies from literature has suggested PCT to be a useful marker in the diagnosis of sepsis [24,25].
CRP values can be used to diagnose an inflammatory condition or infection of newborns, which could develop into sepsis. Increasing values of CRP starts 8 hours after infection [26]. The half-life of CRP is 19 hours [27]. This local production of CRP may be a process of localized inflammation and a marker for local cellular damage. In our study statistical analysis of correlation of positive and negative blood culture confirmed significantly different values of CRP in the analyzed time period. ANOVA test show statistical significance p<0.001 (Figure 5). The highest average values in newborns with positive blood culture were measured (52.72 ± 85.69) after the second measurement on day 3-5, with a subsequent sharp jump compared with newborns with negative blood culture [28,29]. The three CRP measurements can be helpful in monitoring the response to treatment in newborns with sepsis positive and negative blood culture, to determine possible complications to develop severe sepsis and septic shock.
In our study we confirmed that there is no correlation between values of WBC in newborns with sepsis with positive and negative blood culture in the analyzed time period, except at the 14 newborns with severe sepsis and septic shock we confirmed very decreased value of WBC. In the literature these results indicate that leukopenia (WBC<4,000) in severe sepsis newborns leads to more severe outcome than leukocytosis (WBC>12,000) in severe sepsis newborns.
Conclusion
The values of inflammatory markers for sepsis are important clinical significance in predicting the prognosis of newborns with positive and negative blood cultures. We examined three parameters in newborns with proven sepsis, the values of PCT increased at the moment of admission in the group of newborns with positive blood cultures compared with the group of newborns with negative blood culture, while the values of of C-reactive protein gradually increased.
Procalcitonin values are most important diagnostic and early prognostic factor for sepsis in newborns, whose values can prevent the development of severe sepsis and septic shock. It is a reliable biomarker whether an appropriate antibiotic for the treatment is used, thus increasing newborns safety, reducing costs and decreased the development of antibiotic resistance.
References
- Fung AWS, Beriault D, Eleftherios P (2017) The role of procalcitonin in diagnosis of sepsis and antibiotic stewardship: Opportunities and challenges. Clinical Chemistry 63: 1436-1441.
- Becker KL, Snider R, Nylen ES (2010) Procalcitonin in sepsis and systemic inflammation: A harmful biomarker and a therapeutic target. Br J Pharmacol 159: 253-264.
- Sager R, Kutz A, Mueller B, Schuetz P (2017) Procalcitonin guided diagnosis and antibiotic stewardship revisited. BMC Medicine 15: 15.
- Meisner M (2014) Update on procalcitonin measurements. Ann Lab Med 34: 263-273.
- Llewelyn M, Cohen J, International Sepsis Forum (2001) Diagnosis of infection in sepsis. Intensive Care Med 27: S10-32.
- Whicher J, Bienvenu J, Monneret G (2001) Procalcitonin as an acute phase marker. Ann Clin Biochem 38: 483-493.
- Gogos CA, Drosou E, Bassaris HP, Skoutelis A (2000) Pro-versus anti-inflammatory cytokine profile in patients with severe sepsis: A marker for prognosis and future therapeutic options. J Infect Dis 181: 176-180.
- Muller B, White JC, Nylén ES, Snider RH, Becker KL, et al. (2001) Ubiquitous expression of the calcitonin-i gene in multiple tissues in response to sepsis. J Clin Endocrinol Metab 86: 396-404.
- Lee H (2013) Procalcitonin as a biomarker of infectious diseases. Korean J Intern Med 28: 285-291.
- Schneider HG, Lam QT (2007) Procalcitonin for the clinical laboratory: A review. Pathology 39: 383-390.
- Brun-Buisson C (2000) The epidemiology of the systemic inflammatory response. Intensive Care Med 26: S74-S79.
- Black S, Kushner I, Samols D (2004) C-reactive protein. Minireview. J Biol Chem 279: 48487-48490.
- Ng P (2004) Diagnostic markers of infection in neonates. Arch Dis Child Fetal Neonatal Ed 89: 229-235.
- Jensen JU, Heslet L, Jensen TH, Espersen K, Steffensen P, et al. (2006) Procalcitonin increase in early identification of critically ill patients at high risk of mortality. Crit Care Med 34: 2596-2602.
- Kim H, Kim Y, Lee HK, Kim KH, Yeo CD (2014) Comparison of the delta neutrophil index with procalcitonin and C-reactive protein in sepsis. Clin Lab 60: 2015-2021.
- Chiesa C, Panero A, Rossi N (1988) Reliability of procalcitonin concentrations for the diagnosis of sepsis in critically ill neonates. Clin Infect Dis 26: 664-672.
- Vincent JL (2000) Procalcitonin: The marker of sepsis? Crit Care Med 28: 1226-1228.
- Athhan F, Akagunduz B, Genel F, Bak M, Can D (2002) Procalcitonin: A marker of neonatal sepsis. J Trop Pediatr 48: 10-14.
- Carrol ED, Newland P, Riordan FAI, Thomson APJ, Curtis N, et al. (2002) Procalcitonin as a diagnostic marker of meningococcal disease in children presenting with fever and a rash. Arch Dis Child 86: 282-285.
- Carrol ED, Thomson AP, Hart CA (2002) Procalcitonin as a marker of sepsis. Int J Antimicrobe Agents 20: 1-9.
- Schuetz P, Albrich W, Mueller B (2011) Procalcitonin for diagnosis of infection and guide to antibiotic decisions: Past, present and future. BMC Med 9: 107.
- Ugarte H, Silva E, Mercan D, De Mendonça A, Vincent JL (1999) Procalcitonin used as a marker of infection in the intensive care unit. Crit Care Med 27: 498-504.
- Hansson LO, Lindquist L (1997) C-reactive protein: Its role in the diagnosis and follow-up of infectious diseases. Curr Opin Infect Dis 10: 196-201.
- Castelli GP, Pognani C, Meisner M, Stuani A, Bellomi D (2004) Procalcitonin and C-reactive protein during systemic inflammatory response syndrome, sepsis and organ dysfunction. Crit Care 8: R234-R242.
- Pfäfflin A, Schleicher E (2009) Inflammation markers in point-of-care testing (POCT) Analytical and Bioanalytical Chemistry 393: 1473-1480.
- Vigushin DM, Pepys MB, Hawkins PN (1993) Metabolic and scintigraphic studies of radioiodinated human C-reactive protein in health and disease. J Clin Invest 91: 1351-1357.
- Chan Dk, Ho LY (1997) Usefulness of C-reactive Protein in the diagnosis of neonatal sepsis. Singapore Med J 38: 252-255.
- Jave DL, Waites KB (1996) Clinical applications of C-reactive Protien in pediatrics. Pediatr Infect Dis J 16: 735-746.
- Tanaka H, Ikeda T, Ono S, Suda S, Ueno T (2015) White blood cell counts have an impact on septic patient outcome followed by polymyxin-b immobilized fiber with direct hemoperfusion. Crit Care 19: P128.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences