A Deep Esophageal Injury from a Lithium Battery: A Case Report
Barabino AV, Magnano GM, Gandullia P and Leoni M
DOI10.21767/2471-805X.100010
Barabino AV*, Magnano GM, Gandullia P and Leoni M
Gastroenterology and Digestive Endoscopy Unit, Radiology Department, Istituto G. Gaslini (IGG), Genoa, Italy
- *Corresponding Author:
- Arrigo Vittorio Barabino
Head of Gastroenterology and Digestive Endoscopy Unit, G. Gaslini Institute, Via G. Gaslini 5, 16148, Genoa Italy
Tel: +3901056362771
Fax: +39010383688
Received date: December 18, 2015; Accepted date: March 5, 2016; Published date: March 11, 2016
Citation: Barabino AV, Magnano GM, Gandullia P, et al. A Deep Esophageal Injury from a Lithium Battery: A Case Report. J Pediatr Care. 2016, 2:1. doi:10.21767/2471-805X.100010
Abstract
Context: Over the last ten years the ingestion of disk batteries and its serious consequences have been increasing. The severity of injury is related to a growing diffusion of the new lithium battery that may cause catastrophic damages when lodged in the esophagus in children.
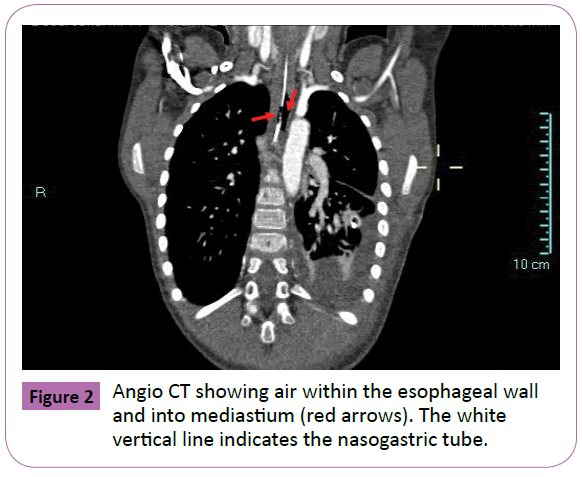
Case report: A five-year-old boy presented to the Emergency Department of our tertiary pediatric Institute for a lithium battery lodged in the mid esophagus. Emergent esophagoscopy revealed a severe deep, mild bleeding ulceration of the wall in which the battery was partially wedged. The investigation was stopped and on-call cardio-vascular surgeon started left thoracotomy to exclude damages of the main vessels. With the thorax open, the endoscopy was repeated and a directional relationship between the battery and the aorta was excluded by means of trans illumination. The cell, a CR2032 lithium battery, was then removed. Central line parenteral nutrition, i.v. omeprazole plus antibiotics were started with a drainage tube left in the chest. During the follow-up the child undergone several chest X-rays with the suspicion of esophageal perforation. Angio-TC done on day 7 showed air into the thickened esophageal wall and in the mediastinum with severe peri-aortic edema without lesion of the vessel. MRi performed on day 21 showed only a persistent thickening of the esophageal wall. On day 28 an esophagogram was normal and the child was discharged asymptomatic. Two months later the investigation was repeated resulting entirely normal.
Conclusion:Treatment of disk battery ingestion requires a multidisciplinary approach that can be implemented only in a tertiary pediatric hospital. Surgery can play an important role. Severe complications can occur several days after battery removal
https://betsatgirisi.com https://bettilte.com https://vegabete.com https://kanyongiris.com https://matgiris.com https://celtabetegiris.com https://hilbetegiris.com https://melbete.com https://kinbettinge.com https://wipbett.com https://pusulabetegiris.com https://superbahiss.com https://lidyagiris.com https://holiganbete.com https://1xbetgiriss.com https://asyabahise.com https://jetbahise.com https://betdoksana.com https://betebetle.com https://betgramagiris.com
Keywords
Lithium battery ingestion; Aorto-esophageal fistula; Esophageal injury; Children
Introduction
The ingestion of disk battery (DB) may cause catastrophic complications, and 44 deaths in children have been reported worldwide so far [1]. Sixty-six percent of them were due to a fistula between esophagus and aorta (AEF) or other major vessels. In order to stop the continuing rise in life-threatening injuries several multi-faceted approaches have been proposed [2-7].
The severity of injury depends on cell type, size, voltage, location and time of tight contact with the mucosa. The main lesion mechanism is an electrical generation of hydroxide ions at the negative pole causing an alkaline burn proportional to the battery voltage. Lithium battery (LB) is larger (> 20 mm), flatter and have a higher voltage (3V) than the alkaline DB (1.5 V). In small children the ingestion of such cells increases the risk of esophageal lodgment and significant tissue damage in just two hours [2,3] if not witnessed ingestion making an early diagnosis is a clinical challenge that has significant implications on primary care setting [8].
Clinical presentation can be extremely variable and difficult to recognize. The child with a DB located in the GI tract can be symptom-free or present typical symptoms such as drooling, dysphagia, vomiting, chest pain or dyspnea. Atypical symptoms are fever, abdominal pain, irritability and feeding refusal. Sudden fatal exsanguination for a fistula between esophagus or other major vessels of the mediastinum can also be a dramatic presentation [4,5].
Other reported complications are: tracheo-esophageal fistula, laryngeal or esophageal stenosis, esophageal perforation, vocal cord paralysis, tracheomalacia, aspiration pmeumonia, empyema, lung abscess and spondylodiscitis [4]. Complications can be delayed, as the mucosal lesions could worsen after cell removal. Plain chest and abdomen X-ray investigations have a primary role to make the diagnosis and to locate the battery that can be recognized by the presence of the double ring or “halo” effect. Urgent endoscopic removal of the DB depends on the clinical presentation.
In 2011 it was documented that a “sentinel bleed”, such as an isolated hematemesis or melena occurring hours or days before a fatal hemorrage, might be another atypical presenting symptom [5]. Exsanguination may occur with the battery still in the GI tract or after its removal. The interval between battery removal and fatal hemorrhage ranges between 2 and 28 days [1,2]. In stable patients with ‘‘sentinel bleeds’’ there is a time window that allows a successful surgical intervention, as suggested by the protocol developed by Brumbaugh and co-workers [5].
Here we describe a child with a LB lodged into the esophagus seen in our tertiary pediatric Institute. He required urgent thoracotomy to exclude aorta involvement suggested by severe ulcerations of the esophagus seen at endoscopy. The outcome was complicated by suspected esophageal perforation fully recovered with conservative treatment.
Case Report
A 5-year-old boy was admitted on September, 2012 for three day history of epigastric pain persisting despite oral omeprazole. The mother reported possible ingestion of a coin. A plain chest and abdomen X-ray showed a LB lodged in mid-oesophagus (Figure 1). No history of previous sentinel bleed was reported and physical examination was unremarkable. Blood tests were normal. The patient, monitored by an anesthesiologist, was immediately transferred to the operating room where the GI endoscopist was ready to remove the battery. Oesophagoscopy (GIF-180 videogastroscope, Olympus, Milan) revealed a severe, deep, mildly bleeding ulceration of the oesophageal wall in which the battery was partially wedged. Oesophagoscopy was stopped, while the anesthesia was continued. Within 25 minutes, the on-call cardiovascular (CV) surgeon started left thoracotomy to exclude damages of the aorta. With the thorax open, an intraoperative assisted endoscopy was done, and a direct contact between the battery and the aorta was excluded by means of transillumination. The battery, a CR2032 LB, was pushed into the stomach and then removed. Central line parenteral nutrition, open naso-gastric tube, i.v. omeprazole, and antibiotics were started. During the follow-up the child undergone several chest X-rays with the suspicion of esophageal perforation. Angio- TC done on day 7 showed air in the thickened esophageal wall and in the mediastinum, with severe peri-aortic edema without lesion of the vessel (Figure 2). MRI performed on day 21 showed only a persistent thickening of the esophageal wall. On day 28 an esophagogram was normal and the child was discharged asymptomatic. Two months later the investigation was repeated resulting entirely normal.
Discussion
In this case the single symptom related to DB stuck in the esophagus was epigastric pain. X-ray was able to correctly differentiate the LB from a coin, recognizing the typical double ring or the halo effect. According to the Brumbaugh’s protocol [5] the child should have been managed by an emergent gastroscopy to immediately remove the cell. Because the severe esophageal lesion was suggestive for a possible involvement of the aorta or other major vessels of the mediastinum, the cell was not touched. Despite the lack of a previous “sentinel bleed”, we wished to avoid the “activation” of an underling AEF with an immediate fatal consequence. At that time the battery could act as a plug of a vessel lesion preventing a major bleeding to occur. According to that the Brumbaugh guideline [5] was not followed, and we chose to exclude vessels damage by thoracotomy. This case underlies the crucial role of the endoscopy in this clinical presentation because the severity of the lesions indicates next operating steps, and induced us to modify the multidisciplinary approach to DB ingestion in children [7].
As reported in the literature several days after the cell removal a suspected esophageal perforation with a peri-aortic severe edema occurred highlighting the potential late consequences of the DB ingestion, requiring a close clinical follow-up by means of traditional radiology, CT scan, MRI or repeating endoscopy.
References
- National Capital Poison Center: https://www.poison.org/battery/fatalcases.asp
- Jatana KR, Litovitz T, Reilly JS(2013)Pediatric button battery injuries: 2013 task force update. International Journal of Pediatric Otorhinolaryngology77:1392–1399.
- Litovitz T, Whitaker N, Clark L (2010)Preventing battery ingestions: an analysis of 8648 cases. Pediatrics125: 1178-1783.
- Litovitz T, Whitaker N, Clark L (2010) Emerging battery ingestion hazard: clinical implications. Pediatrics 125:1168–1677.
- Brumbaugh DE, Colson SB, Sandoval JA(2011) Management of button battery–induced haemorrhage in children. J Pediatr Gastroenterol Nutr 52:585–589
- Rossi A, Barabino A, Vignola S, Bini M (2015) Lithium disk battery: the silent killer. J Gastroenterol Hepatol Res 4:1624-1634
- Kramer RE, Lerner GD, Lin T (2015) Management of ingested foreign bodies in children: a clinical report of the NASPGHAN Endoscopy Committee. J Pediatr Gastroenterol Nutr 60:562-574
- Shepherd M, Hamill JK, Barker RJ (2014)Buttonbattery injury in children - a primary care issue? Prim Health Care. 6:69-72.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences