A cost-effectiveness analysis of inpatient telemedicine pediatric consults in satellite hospitals.
*Anirudha Das MD1, Chionye Ossai MD1, Ajith Mathew MD1
*Anirudha Das MD, Chionye Ossai MD, Ajith Mathew MD
Departmemt of Neonatology, Cleveland Clinic,United States
*Corresponding Author: Dr. Anirudha Das MD, Children & Adolescents doctor, Departmemt of Neonatology, Cleveland Clinic, United States; Tel: 8639887943; E-Mail: anirudhdas26@gmail.com
Received date: October 14, 2020; Accepted date: August 17, 2021; Published date: August 27, 2021
Citation: Anirudha Das MD (2021) A cost-effectiveness analysis of inpatient telemedicine pediatric consults in satellite hospitals. J Pediatr care 7.no.4.
Abstract
Telemedicine has been growing in popularity in pediatric health care. Convenience of use, efficiency and limited need for resources are the primary drivers but barriers remain in widespread acceptance due to provider apprehension and inconsistent reimbursement. The onset of the global COVID-19 pandemic and associated need for social distancing has changed the telemedicine landscape drastically as government and providers scramble to telemedicine as an alternative to continue to evaluate and manage patients safely. With the limitations in mind, telemedicine has not only been shown to be cost effective but may also contribute to curb climate change. In large hospital networks, subspecialists mostly prefer to travel from the main hospital to the satellite locations to do consults driven partly by the need for higher reimbursement amount and partly from discomfort with the use of novel technology. We present a model for pediatric inpatient consults and compare its cost- effectiveness to face-to-face consultation in our hospital system.
https://betkolikgirisi.com https://betlikeguncel.com https://betparkagiris.com https://bettickett.com https://betturkeyegiris.com https://extrabetgirisi.com https://holiganbeti.com https://ilbete.com https://ikimisligirisi.com https://imajbetegir.com https://jojobeti.com https://kralbetting.com https://mariogiris.com https://marsbahise.com https://meritegiris.com https://milanobeti.com https://piabetegir.com https://redwinegiris.com https://supertotobete.com https://tempobetegir.com
Background
Telemedicine has been growing in popularity in pediatric health care. Convenience of use, efficiency and limited need for resources are the primary drivers but barriers remain in widespread acceptance due to provider apprehension and inconsistent reimbursement. The onset of the global COVID-19 pandemic and associated need for social distancing has changed the telemedicine landscape drastically as government and providers scramble to telemedicine as an alternative to continue to evaluate and manage patients safely. With the limitations in mind, telemedicine has not only been shown to be cost effective but may also contribute to curb climate change. In large hospital networks, subspecialists mostly prefer to travel from the main hospital to the satellite locations to do consults driven partly by the need for higher reimbursement amount and partly from discomfort with the use of novel technology. We present a model for pediatric inpatient consults and compare its cost-effectiveness to face-to-face consultation in our hospital system.
Methods
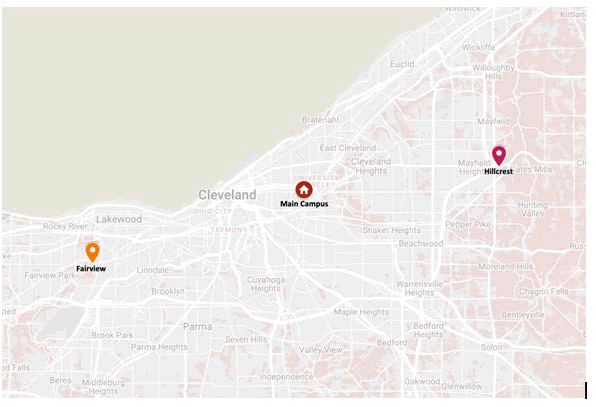
Pediatric subspecialists from the main campus (MC) of the Cleveland Clinic hospital system have traditionally traveled to the satellite centers - Fairview (FV) and Hillcrest (HL) hospitals to consult in-person on pediatric cases. For travel between MC and HL hospitals (10.4 miles), in a car, back and forth, including time spent at bedside and documentation (30 minutes), it takes approximately 1 hour 30 minutes in average traffic conditions, traveling by passenger car with average mileage, while for FV hospital it takes almost similar time although the distance is greater (14 miles) (Figure 1). Traveling to HL for a face-to-face consultation generates 4.2 kilograms (kgs) of carbon dioxide equivalent (CO2e)emission, per visit, from an average passenger vehicle and about 5.6 kgs for FV 4,5,6. The average pediatric subspecialty professional charge for such a visit is $673.00. After subtracting the travel expenses per mile (55 cents) the total amount billed for each visit is $667.50 for HL and $665.30 for FV. Comparatively, a telemedicine visit is not being billed for professional charges to the insurance company at the time of writing this evaluation although providers get 1.92 relative value unit (RVU) credits for a new 30-minute visit. The hour of travel time saved could be utilized by the subspecialist to perform at least 2 outpatient visits of 20 minutes each at the MC, a total of $856 ($428 each), calculated to $846 after deducting the cost of telemedicine platform (average $7/use) usage and internet/electricity/equipment fee (considered to be $3/use). Thus, using telemedicine could potentially offset the cost of the face-to-face visit and save $178.5 and $180.7 for every consultation to HL and FV respectively.
Results
In 2019, 85 inpatient regional consults were conducted in the children’s hospital. Let us compare these 85 telemedicine consults with physical consults in our cost-effectiveness analysis. In financial terms, those virtual visits could have potentially saved $7140 (40 consults X $178.5) for the HL and $8131.50 (45 consults X $180.7) for FV annually. The telemedicine visits could also potentially have reduced CO2e emission by 168 kgs for HL and 252 kg for FV, a total of 420 kgs of CO2e emission for the entire year. This is equivalent to the carbon sequestered by 0.549 acres of trees in a year. The damaging impacts on health are estimated by using the IMPACT2002+ life cycle impact assessment model, multiplying the yearly emission by “characterization factor”, which represents its fate, potential exposure, and the effect of that exposure, based on physical-chemical and toxicological data. According to the model, the estimate of health outcome calculated for CO2e is a median of 1092 Disability adjusted life years (DALY) lost annually with an uncertainty range of 42 – 73,920 DALYs 7,8. Considering the population of Cleveland (383,793, US census Bureau) with a life expectancy of 78.5 years (United States, World Bank data), the average increment of days, when telemedicine consults are utilized, without disability, ill-health or premature death is calculated to be 2 months and 18 days per individual in their lifetime.
Discussion
The CEA was able to demonstrate that pediatric consults for the regional hospitals using telemedicine would not only be economically preferable but also beneficial to health. This model shows that although the impact of telemedicine for a single department with limited use is minor, the potential wider use of telemedicine will have an exponential impact on the environment and ultimately our health. Physical examination is one of the limitations of telemedicine but virtual examination with the help of the remote end user provider in the regional hospitals have been proven to be reliable with or without enhancements such as electronic stethoscopes, tele-ophthalmoscopes and derma scopes 9,10,11,12. High resolution models have previously found that emission induced temperature rise may increase U.S. annual air pollution related deaths by about 1000 (350–1800) andcancers by 20–30/1000 13. Wider use of telemedicine can reduce emissions and improve health.
There are several limitations. Provider familiarity, ease of use and effective utilization of the technology were not considered in the model. Only standard passenger cars were considered, and route of transportation was calculated to and from the main hospital without any exceptions which could lead to inaccuracies. The wide uncertainty range makes it difficult to accurately measure the health impact which is another limitation.
Conclusion
Based on our model, the 85 telemedicine consultations could potentially save 15,271.50 dollars/year for the hospital system and reduce DALYs by 1092 (median) per year in the local population. The exponential growth of telemedicine due to the pandemic is the right opportunity for a paradigm shift in the use of this technology for economic and health benefits demonstrated by this analysis.
Author disclosure statement
Dr. Das, Dr. Ossai and Dr. Mathew hereby declare that they have no financial relationships or conflicts of interest relevant to this article to disclose.
Legend
References
- Ratageri VH, Shepur TA, Wari PK, Chavan SC, Mujahid IB, Yergolkar PN et al. (2005) Profile and outcome of dengue fever cases. Indian J Pediatr.72:7 05â??6
- Narayanan M, Aravind MA, Thilothammal N, Prema R, Sargunam CS, Ramamurty N et al. (2002) Dengue fever outbreak in Chennaiâ??A study of clinical profile and outcome. Indian Pediatr 39:10 27â??33
- Lopez GL, Anderson KH, Feutchinger J. (2012) Transition of premature infants from hospital to home life. Neonatal Netw 31:4.
- Discenza D. (2009) NICU parentsâ?? top ten worries at discharge. Neonatal Netw. 28:3
- Kuppala VS, Tabangin M, Haberman B, Steichen J, Yolton K. et al. (2012) Current state of high-risk infant follow-up care in the United States: Results of a national survey of academic follow-up programs. J Perinatol. 32:293â??298
- Bockli K, Andrews B, Pellerite M, Meadow W. (2014) Trends and challenges in United States neonatal intensive care units follow-up clinics. J Perinatol. 34:71â??74.
- Lantos J. (2010) Cruel calculus why saving premature babies is better business than helping them thrive. Health Aff. 29:2114â??2117.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences